Vancomycin Infusion Rate Calculator
Safe Infusion Time
Enter a dose to calculate minimum infusion time.
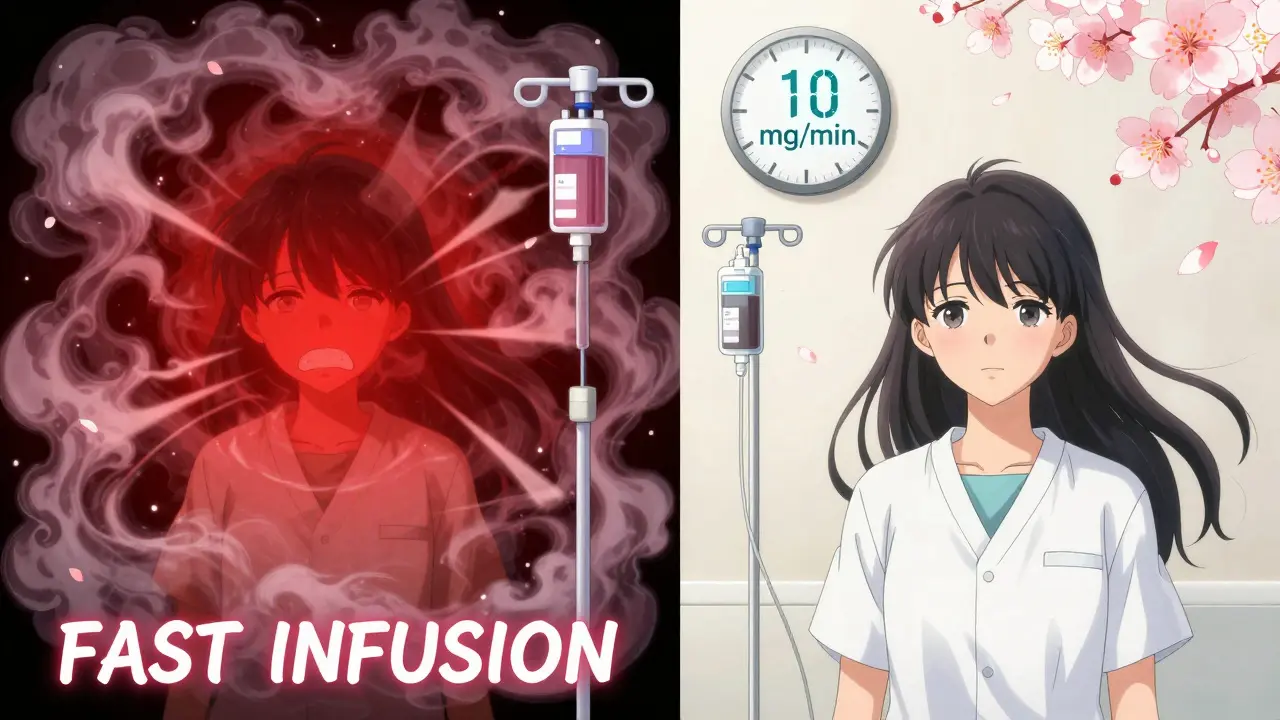
Important: Infuse vancomycin at 10 mg/min or slower to prevent infusion reactions. The calculator shows the minimum time required to stay below this rate.
Vancomycin is a powerful antibiotic used to treat serious bacterial infections like MRSA and severe Clostridioides difficile. But if it’s given too fast, it can trigger a reaction that turns skin red, makes you itch, and drops your blood pressure. For years, this reaction was called red man syndrome-a term now widely recognized as outdated and offensive. Today, medical professionals call it vancomycin infusion reaction or vancomycin flushing syndrome. The name change isn’t just about politeness-it’s about accuracy. This isn’t a true allergy. It’s a predictable, preventable reaction tied to how quickly the drug enters your bloodstream.
What Actually Happens During a Vancomycin Infusion Reaction?
When vancomycin is infused too rapidly-faster than 10 mg per minute-it directly triggers mast cells and basophils in your body to dump histamine. This isn’t an immune system response like a peanut allergy. You don’t need to have been exposed before. It happens the first time, and it can happen every time if you don’t slow the drip.
Within 15 to 45 minutes of starting the infusion, you might notice your face, neck, and upper chest turning bright red. It’s not a rash you can scratch off-it’s flushing, like a bad sunburn that spreads. Along with the redness comes intense itching, a feeling of warmth, and sometimes a pounding headache. In more severe cases, your heart races, your blood pressure drops, and you might feel chest tightness or muscle spasms. Breathing problems? Rare. That’s a sign of something else, like true anaphylaxis.
Studies show this reaction is almost guaranteed if you get a full gram of vancomycin in under an hour. One 1988 study found 9 out of 11 healthy adults developed symptoms under those conditions. But when the same dose was given over 2 hours? Zero reactions. The data is clear: speed kills-literally, in this case.
Why the Name Changed: From ‘Red Man Syndrome’ to Vancomycin Infusion Reaction
The term ‘red man syndrome’ wasn’t just misleading-it was harmful. It implied the reaction only happened to men, and worse, it used a racial stereotype to describe a physiological event. In 2021, researchers at a major children’s hospital reviewed over 21,000 patient records and found that 61.6% of vancomycin allergy notes still used the old term. That meant patients were being labeled as allergic to vancomycin when they weren’t-just because they’d flushed during an infusion.
After switching all records to use ‘vancomycin flushing syndrome’ and training staff on the correct terminology, the use of the old term dropped by 17% in just three months. Hospitals like UCSF now require all staff to use ‘vancomycin infusion reaction’ in charts, prescriptions, and verbal reports. The Infectious Diseases Society of America officially recommends this change. Why? Because mislabeling a reaction as an allergy can lead to patients being denied effective antibiotics. If a doctor thinks you’re allergic to vancomycin, they might give you something less effective, more toxic, or more expensive-just because of a misnamed side effect.
How to Tell It’s Not a True Allergy
True allergic reactions to vancomycin are rare-only about 3% of patients labeled as allergic actually have one. Most of those cases involve serious skin conditions like DRESS, Stevens-Johnson Syndrome, or toxic epidermal necrolysis. These are life-threatening and require immediate stopping of the drug and hospital care.
Vancomycin infusion reaction? It’s different. You won’t get swelling of the tongue or throat. You won’t wheeze. Your lungs stay clear. The redness stays above the waist. Symptoms start during the infusion and fade within 30 minutes after stopping it. And here’s the kicker: if you’ve had it once, you’re less likely to get it again. The body seems to adapt. That’s called tachyphylaxis. It’s not immunity-it’s just your cells getting tired of releasing histamine.
Other drugs can cause similar flushing: amphotericin B, rifampin, and even some fluoroquinolones like ciprofloxacin. But they work through different mechanisms. Amphotericin B triggers the complement system. Rifampin creates reactive chemicals that bind to your cells. Vancomycin? It just hits mast cells directly. That’s why slowing the drip works every time.

How to Prevent It: The Simple Rules
Preventing vancomycin infusion reaction isn’t complicated. It’s about time and patience.
- Infuse 1 gram of vancomycin over at least 60 minutes. Better yet, stretch it to 90-120 minutes.
- Never go faster than 10 mg per minute. That’s the red line.
- Don’t mix vancomycin with other drugs that trigger histamine release-like opioids (morphine, fentanyl), muscle relaxants, or IV contrast dye.
- Don’t pre-medicate with antihistamines unless you’ve had a prior reaction. There’s no need to give diphenhydramine to someone who’s never had a flush. It adds cost, risk, and doesn’t help.
One hospital in California tracked over 1,000 vancomycin infusions after enforcing the 10 mg/min rule. The rate of reactions dropped from 38% to less than 2%. That’s not luck-that’s protocol.
What to Do If a Reaction Happens
If you’re getting an infusion and feel your face getting hot, your skin burning, or your chest tightening, tell the nurse immediately. Stop the drip. Don’t wait. Don’t assume it’s ‘just a reaction’ and keep going.
The nurse should:
- Stop the vancomycin infusion right away.
- Check your vital signs-blood pressure, heart rate, oxygen levels.
- Notify the provider on call.
- Keep you lying down and monitor you for 30-60 minutes.
Most reactions resolve on their own. But if your blood pressure drops, you might need fluids or a medication like epinephrine. In rare cases, you’ll need to be moved to a higher level of care.
After the episode, your medical team should document it correctly: vancomycin infusion reaction, not allergy. That way, future providers know you can still safely take vancomycin-just slower.
When You Really Can’t Use Vancomycin
There are times when vancomycin isn’t safe at all. If you’ve had a true IgE-mediated allergic reaction-hives, swelling, trouble breathing, anaphylaxis-then you need a different antibiotic. Alternatives include linezolid, daptomycin, or ceftaroline, depending on the infection.
For patients who need vancomycin but keep having reactions even at slow rates, doctors can try desensitization. This is a slow, controlled process done in a hospital setting where tiny doses are given over hours, gradually building tolerance. It’s not for everyone, but it works for some.
And if you’re on vancomycin and you’re also getting pain meds or muscle relaxants? Ask if they can be held during the infusion. Combining them increases the chance of a reaction. Simple fix. Big impact.
Bottom Line: It’s Not an Allergy. It’s a Dose Problem.
Vancomycin is a lifesaver. But like many powerful tools, it has rules. Infuse it too fast, and your body reacts. Infuse it right, and it works without a hitch. The old term ‘red man syndrome’ made it sound mysterious, unpredictable, even dangerous in a way that scared patients and doctors alike. The truth? It’s predictable. It’s preventable. And it’s not your fault.
Next time you hear someone say ‘red man syndrome,’ correct them gently. Say ‘vancomycin infusion reaction.’ It’s not just semantics. It’s better care. It’s safer care. And it’s the standard now.

Ryan Pagan
January 29, 2026 AT 11:47Vancomycin infusion reactions are one of those things that should be taught in med school on day one, but somehow still get botched in 2024. I’ve seen residents rush it because they’re ‘in a hurry’-and then the patient turns into a lobster. Slowing it down isn’t just protocol, it’s basic respect for the drug and the patient. And yes, the term ‘red man syndrome’ was always ridiculous. It’s not about being PC-it’s about being accurate. The body doesn’t care about your race, it cares about your infusion rate.
DHARMAN CHELLANI
January 30, 2026 AT 14:37lol so now we cant say red man syndrome but we can say ‘flushing syndrome’ like its a spa treatment? next theyll call a heart attack ‘chest discomfort episode’
Alex Flores Gomez
January 30, 2026 AT 22:09Actually the term 'red man syndrome' was never offensive-it was just descriptive. They're erasing language to make people feel better, not to fix the problem. And don't get me started on how hospitals now give benadryl like candy before every dose. It's overmedication disguised as caution.
Megan Brooks
January 31, 2026 AT 08:35I appreciate how this post clarifies the distinction between true allergy and infusion reaction. Too often, patients are labeled 'allergic' based on a single episode of flushing, and then they’re denied effective treatment. The shift in terminology isn’t performative-it’s clinical. And the data showing near-elimination of reactions with slower infusions? That’s evidence-based medicine at its best. Let’s keep pushing for precision in language and practice.
Pawan Kumar
February 1, 2026 AT 10:47One must wonder: if the medical establishment is so concerned with linguistic sensitivity, why are they still using terms like 'anaphylaxis'-a Greek word rooted in ancient superstition? Or 'gout'-from Latin 'gutta' meaning 'drop'? The entire lexicon of medicine is steeped in archaic, culturally loaded terminology. The fixation on 'red man syndrome' is a distraction from deeper systemic failures: understaffed units, rushed protocols, and the commodification of patient care. This isn’t about language-it’s about power. Who gets to name suffering? And who profits from the confusion?
rajaneesh s rajan
February 2, 2026 AT 03:33So basically, if you’re getting vancomycin and your face turns red, just chill, tell the nurse, and slow it down. No biggie. But if you say ‘red man syndrome’ out loud, suddenly you’re a villain? I mean… it’s just a phrase. People aren’t idiots. They know it’s not about race. They just like saying it because it’s catchy. Maybe instead of policing words, we should police infusion pumps that don’t have speed alarms. Fix the machine, not the meme.
paul walker
February 3, 2026 AT 14:52just had this happen to me last week. stopped the drip, got a blanket, felt better in 20 mins. doc wrote 'allergy' anyway. i had to ask twice to fix it. why is this still so hard??
kabir das
February 4, 2026 AT 19:39And yet... they still mix vancomycin with vancomycin? No-wait-I mean, they still mix it with morphine?!! And then wonder why patients are red?!! And then blame the patient for being 'sensitive'?!! And then chart it as 'allergy'?!?! And then deny them life-saving antibiotics?!?! And then wonder why mortality rates are rising?!?! And then... oh wait... they don’t wonder. They just bill for the extra ICU stay. That’s the real syndrome here.
ryan Sifontes
February 5, 2026 AT 12:02they changed the name so now im not allergic but i still get red. so what do i tell the er next time? i dont know anymore