When you pick up your prescription, you might not notice that the pill looks different this time. Maybe it’s a different color, shape, or has a new imprint. That’s not a mistake-it’s generic switching. More than 90% of prescriptions in the U.S. are filled with generic drugs, and you’re likely to get a different manufacturer’s version each time you refill. For most people, this is harmless. But for some, it can be dangerous.
Why Do Generic Switches Happen?
Generic drugs are cheaper copies of brand-name medicines. Once a brand’s patent expires, multiple companies can make the same drug using the same active ingredient. Insurance companies and pharmacies often choose the cheapest option available, which changes frequently. One month you might get Teva’s version of levothyroxine; the next, it’s Mylan’s. Then Sandoz. It’s not about your health-it’s about cost.Pharmacies don’t always tell you when the manufacturer changes. In fact, a 2023 survey found that 62% of doctors didn’t know their patients had been switched until the patient came in with problems. You might think, “It’s the same drug,” and you’re right-technically. But the body doesn’t always see it that way.
Not All Generics Are Created Equal
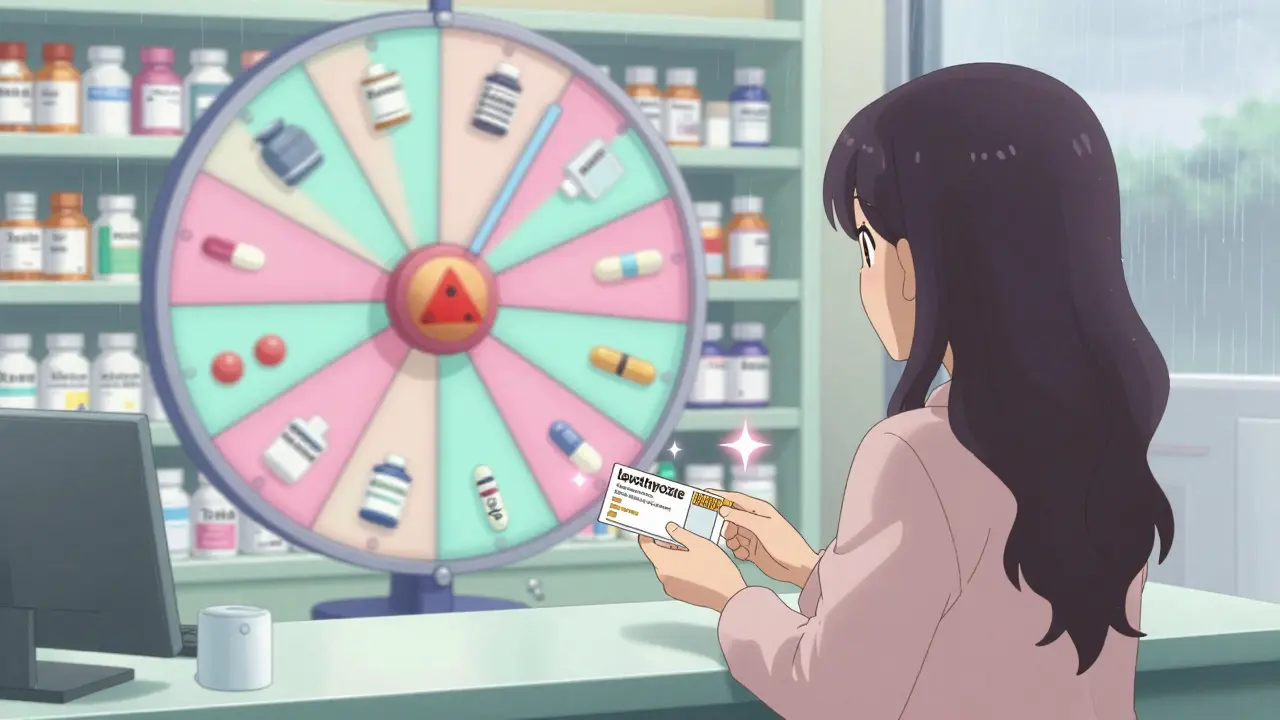
The FDA requires generics to be bioequivalent to the brand-name drug. That means the amount of active ingredient in your blood should be between 80% and 125% of the brand’s level. Sounds fine, right? But here’s the catch: two different generics could be at opposite ends of that range. One might deliver 82% of the active ingredient. Another might deliver 123%. That’s a 41% difference between two pills that are both “approved.”For most medications-like statins or blood pressure pills-this variation doesn’t matter. Your body adjusts. But for drugs with a narrow therapeutic index (NTI), even small changes can cause serious problems.
High-Risk Drugs: When Switching Can Be Dangerous
NTI drugs have a tiny window between being effective and being toxic. A little too little? The condition comes back. A little too much? You could end up in the hospital.Levothyroxine (for hypothyroidism) is one of the most common offenders. Patients report feeling exhausted, gaining weight, or having brain fog every time their pharmacy switches manufacturers. Their TSH levels swing out of range, and it takes weeks to stabilize again. Medsafe, New Zealand’s medicines regulator, explicitly advises against switching brands of levothyroxine unless absolutely necessary.
Warfarin (a blood thinner) is another high-risk drug. A change in generic manufacturer can cause your INR (a measure of blood clotting) to spike or drop. Some studies show increased bleeding or clotting events after switches. Others say there’s no difference. The truth? It varies by person. Many doctors now ask pharmacists to note the manufacturer on warfarin prescriptions-and some hospitals have “lock-in” programs to keep patients on the same version.
Antiepileptic drugs like phenytoin or carbamazepine are the most problematic. One Reddit user shared that after switching from Mylan to Teva, they had two breakthrough seizures. Their neurologist confirmed their blood levels dropped. Studies show 20-44% of epilepsy patients switch back to the original generic-or even the brand-after a change.
What About the Other 70% of Patients?
Most people don’t notice a thing. If you’re on generic lisinopril for high blood pressure, or generic atorvastatin for cholesterol, you’re probably fine. A review of over 1,200 patient reviews found that 68% reported no issues with generic switching. Many people have switched manufacturers five or ten times without any side effects.Why the difference? It comes down to the drug, the person, and how tightly their condition is controlled. If your condition is stable and your drug isn’t in the NTI category, you’re likely safe. But if you’re on a high-risk medication-or you’ve ever had a problem after a switch-you need to pay attention.
How to Protect Yourself
You can’t control which generic your pharmacy dispenses-but you can control how you respond.- Check the pill. Keep a photo of your pill on your phone. If it looks different, ask the pharmacist: “Is this the same manufacturer as last time?”
- Ask for a specific brand. If you’ve had issues before, ask your doctor to write “Dispense as written” or “Do not substitute” on your prescription. This legally prevents the pharmacy from switching without your doctor’s approval.
- Monitor symptoms. If you’re on levothyroxine, warfarin, or an antiepileptic, pay attention to how you feel for two to four weeks after a switch. Fatigue, dizziness, mood changes, or new side effects? Call your doctor.
- Get tested. For NTI drugs, ask your doctor to check blood levels after a manufacturer change. A simple INR test for warfarin or TSH for thyroid meds can catch problems early.
- Use one pharmacy. If you use the same pharmacy every time, they’re more likely to keep you on the same manufacturer. If you switch pharmacies, you increase your risk of a random switch.

What’s Being Done About It?
The problem is growing. In 2023, there were an average of 4.3 generic manufacturers for each off-patent drug in the U.S. That number is rising. The FDA is starting to take notice. In 2023, they launched a pilot program requiring manufacturers to report any formulation changes. In 2024, Medsafe updated its guidelines to discourage levothyroxine switches. The Generic Pharmaceutical Association is working on standardized pill designs to reduce confusion.But the real solution? More transparency. Patients should know which manufacturer made their drug. Pharmacists should be required to tell you. Doctors should be notified. Right now, the system is designed for cost savings-not patient safety.
Bottom Line: Know Your Meds
Generic drugs save billions every year. They’re safe for most people. But assuming all generics are identical is dangerous. If you’re on a high-risk medication, don’t wait for a problem to happen. Be proactive. Ask questions. Track changes. Know your pill. And if you feel off after a switch-don’t brush it off. It might not be “just in your head.” It might be your blood levels.Your health isn’t a commodity. And your medication shouldn’t be treated like a commodity either.
Can I ask my pharmacist to give me the same generic manufacturer every time?
Yes. You can ask your pharmacist to keep you on the same manufacturer. Some pharmacies will honor this request, especially if you explain you’ve had issues before. For high-risk drugs like levothyroxine or warfarin, your doctor can write “Dispense as written” on the prescription, which legally prevents substitution.
Are generic drugs less effective than brand-name drugs?
Not necessarily. Generic drugs must meet the same FDA standards for quality, strength, and purity as brand-name drugs. But effectiveness can vary between different generic manufacturers due to differences in inactive ingredients, absorption rates, and manufacturing processes. For most drugs, this doesn’t matter. For drugs with a narrow therapeutic index, it can.
Why do pharmacies switch generic manufacturers so often?
Pharmacies switch to the lowest-cost option available at the time of refill. Insurance companies and pharmacy benefit managers often require the cheapest generic, which can change weekly based on pricing deals, supply shortages, or new bids from manufacturers. It’s not about your care-it’s about cost control.
What should I do if I think a generic switch caused side effects?
Don’t ignore it. Contact your doctor right away. Keep a log of when you switched, what symptoms started, and how long they lasted. For high-risk drugs like thyroid meds or blood thinners, ask for a blood test to check your levels. You can also report the issue to the FDA’s MedWatch program. Your report helps improve safety for others.
Is it safe to switch between generics for antibiotics or pain relievers?
Yes. For drugs like amoxicillin, ibuprofen, or omeprazole, switching between generics is generally safe. These drugs have wide therapeutic windows, meaning small differences in absorption don’t affect outcomes. Most patients never notice a change. The real concern is with narrow therapeutic index drugs-like thyroid meds, seizure drugs, and blood thinners.

Dana Termini
January 5, 2026 AT 22:39I’ve been on levothyroxine for 12 years and switched manufacturers six times. Three of those times, I felt like a zombie for weeks-brain fog, weight gain, zero energy. My endo finally listened when I brought lab results showing my TSH jumped from 2.1 to 7.8. Now I insist on the same brand. It’s not paranoia-it’s survival.
Pavan Vora
January 7, 2026 AT 07:04Wow, this is so true… I mean, in India, we don’t even get to choose, right? But I had a friend who was on warfarin, and after a switch, she had a mini-stroke… the doctor said it was likely due to INR fluctuation. Pharma companies care about profit, not people. And yes, I know, generics save money-but not if you end up in ICU.
Stuart Shield
January 9, 2026 AT 05:14Man, this hits hard. I used to think generics were just cheaper versions of the same thing-until my cousin, who’s got epilepsy, had three seizures after a switch from Teva to Mylan. His neurologist said it’s like swapping out the engine in your car with one that’s ‘technically the same’ but runs on a different fuel. The FDA’s 80-125% window? That’s not a range-it’s a roulette wheel.
And don’t even get me started on pharmacies not telling you. I once had to call three pharmacies before one admitted they’d switched my mom’s lisinopril. No warning. No note. Just a different-looking pill. That’s not healthcare-that’s a gamble.
Ashley S
January 9, 2026 AT 21:31So people are mad because their pills look different? Grow up. If you can’t tell the difference between a blue pill and a white pill, maybe you shouldn’t be managing your own meds.
Jeane Hendrix
January 11, 2026 AT 13:08As a pharmacist’s assistant, I see this daily. The real issue isn’t bioequivalence-it’s the lack of standardization in inactive ingredients. Fillers, binders, dyes-they vary wildly between manufacturers and can affect absorption, especially in patients with GI issues or allergies. And no, pharmacists aren’t required to log or notify you. It’s a systemic failure. I’ve personally flagged over 200 switches in the last year. Most docs don’t even check.
Also, ‘Dispense as written’ works, but only if your doctor knows to write it. Too many still assume ‘generic = interchangeable.’ They’re not trained in pharmacokinetics. We need mandatory manufacturer labeling on scripts. Like, the name right on the Rx. Not just in the system.
Kelly Beck
January 13, 2026 AT 04:25Y’all, I just want to hug everyone who’s been through this. 💪❤️ Seriously-this is such an important topic and I’m so glad someone finally put it out there. If you’ve ever felt off after a pill change, you’re not crazy. You’re not overreacting. You’re paying attention-and that’s a superpower. Keep tracking your symptoms. Keep asking for blood tests. Keep telling your doctor. Your voice matters. And if your pharmacy gives you grief about sticking with one brand? Tell them you’re not a lab rat. You’re a human. 🌱
Beth Templeton
January 14, 2026 AT 14:26Wow. A 41% difference between generics. And we wonder why people are sick. Next they’ll tell us all McDonald’s burgers are the same.
Cam Jane
January 15, 2026 AT 04:33Just want to add-this isn’t just about pills. It’s about trust. You take your meds every day because you believe they’ll work. Then one day, your body starts acting weird and you’re told, ‘It’s the same drug.’ But your body knows better. I’ve been on carbamazepine since I was 16. Switched once-had a seizure in the grocery store. Never again. I now have my script stamped ‘DO NOT SUBSTITUTE’ and I carry a photo of my pill in my wallet. It’s not extreme. It’s necessary.
And if you’re on a high-risk med? Don’t wait for disaster. Ask your doc to write it. Call your pharmacy and ask which maker they’re using. Keep a log. Share this post. The system won’t fix itself. We have to push.
Indra Triawan
January 16, 2026 AT 19:28Isn’t it ironic? We live in a world where we can track our sleep cycles and optimize our microbiome, yet we’re still handing over our lives to pharmaceutical supply chains that operate like a game of musical chairs? We’ve lost the sacredness of medicine. It’s no longer about healing-it’s about efficiency. And efficiency, my friends, is the new religion.
Susan Arlene
January 17, 2026 AT 12:00My mom’s on warfarin. Switched generics last year. INR went from 2.4 to 4.8 in two weeks. She almost bled out. Now she only gets her script from one pharmacy and only takes the same brand. No drama. No fuss. Just don’t switch. Simple.