Steroid eye drops are powerful tools for treating eye inflammation, but they’re not harmless. If you’ve been prescribed them for uveitis, severe allergies, or injury-related swelling, you need to understand both how they help and what they can do to your eyes over time. These aren’t just ordinary drops-they’re medicine with serious side effects if used too long or without proper oversight.
What Steroid Eye Drops Do
Steroid eye drops, like prednisolone acetate (Pred Forte, Omnipred) and loteprednol etabonate, work by shutting down inflammation at the cellular level. They block enzymes like phospholipase A2 and stop the production of prostaglandins, which are chemicals that cause redness, swelling, and pain in the eye. For conditions like acute anterior uveitis, where inflammation can blur vision or damage the retina, these drops can be life-changing. Many patients see improvement within days. Dr. Daniel Bintz, an optometrist and former chair of the American Optometric Association’s Health Promotions Committee, says patients with uveitis often respond dramatically-sometimes going from barely seeing to reading again after just a week of treatment.
But here’s the catch: they work too well. By suppressing inflammation, they also weaken your eye’s natural defenses. That’s why these drops are never meant to be used for months on end. The goal is always to get the inflammation under control as quickly as possible, then stop or reduce the dose.
The Hidden Dangers: Glaucoma and Cataracts
The biggest risks from steroid eye drops aren’t obvious at first. You won’t feel your eye pressure rising. You won’t notice your lens slowly clouding. That’s why these side effects sneak up on people.
Elevated intraocular pressure (IOP) is the most common danger. About 30-40% of people experience some increase in eye pressure when using steroid drops. For most, it’s mild and goes away when they stop. But 4-6% of users are "steroid responders"-their pressure spikes by more than 15 mmHg. That’s enough to damage the optic nerve over time, leading to glaucoma. And once the nerve is damaged, it doesn’t heal. Vision loss from steroid-induced glaucoma is permanent.
Then there’s cataracts. Long-term use-usually 10 days or more-can trigger posterior subcapsular cataracts. Unlike age-related cataracts that form slowly over years, steroid-induced ones develop quickly, right in the center of your vision. This means blurry vision, glare from lights, and trouble seeing at night. Studies show that people on steroid drops for 3-6 months are at much higher risk of needing cataract surgery years earlier than they otherwise would.
And it gets worse. Steroids also make your eyes more vulnerable to infections. Herpes simplex in the eye, fungal keratitis, and other serious infections can flare up because your immune system is suppressed. These infections can destroy the cornea in days if not caught early.
Who’s at Highest Risk?
Not everyone reacts the same way. Certain people are far more likely to have bad side effects:
- People with a family history of glaucoma
- Those already diagnosed with glaucoma
- Patients with diabetes
- Anyone who’s used steroid drops before and had pressure spikes
- Users of high-potency drops like prednisolone acetate (not low-potency ones like loteprednol)
If you fall into one of these groups, your eye doctor should be extra careful. You might need more frequent check-ups, lower doses, or alternative treatments.

How Often Should You Get Checked?
Monitoring isn’t optional-it’s mandatory. The American Academy of Ophthalmology recommends:
- Measure your eye pressure before you start the drops
- Check again after 2 weeks
- Then every 2-4 weeks if you’re on steroids for longer than 2 weeks
- For high-risk patients, check every 1-2 weeks
These aren’t just routine visits. Each one includes a slit-lamp exam to look for early signs of cataracts and a tonometry test to measure pressure. Goldmann applanation tonometry is the gold standard-it’s the most accurate way to catch rising pressure before it damages your optic nerve.
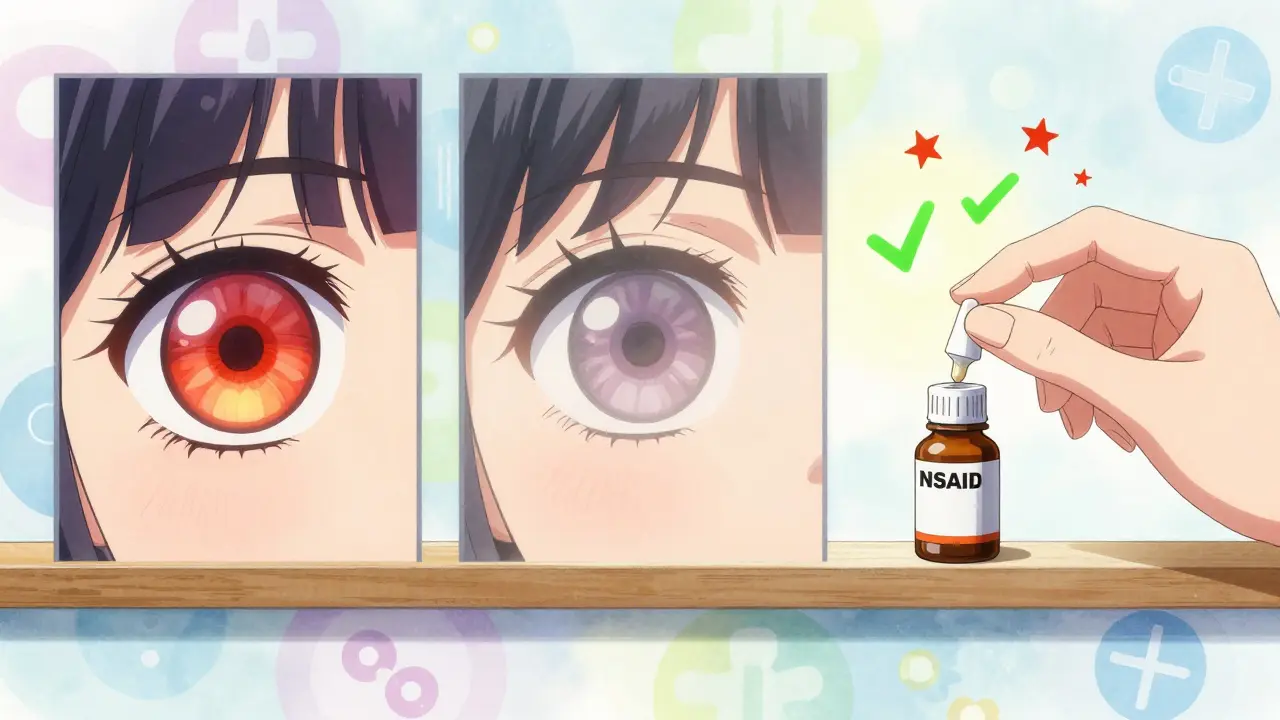
If you’re using steroid drops for more than 4 weeks, your doctor should be seriously considering alternatives. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ketorolac eye drops can help with milder inflammation without the same risks. They don’t work as fast or as strong as steroids, but they’re safer for long-term use.
How Long Is Too Long?
There’s no single answer, but most experts agree on this:
- Less than 2 weeks: Low risk for most people
- 2-4 weeks: Moderate risk, especially with high-potency drops
- More than 4 weeks: High risk for glaucoma and cataracts
- More than 3 months: Very high risk-consider switching treatments
Dr. Bintz says most uveitis patients only need steroids for 1-2 months. After that, the benefit drops off while the risk climbs. If your doctor plans to keep you on them longer, they should have a clear reason-and a backup plan.
Symptoms to Watch For
You might not feel anything until it’s too late. But if you notice any of these, call your eye doctor immediately:
- Blurry vision that doesn’t go away
- Eye pain or pressure
- Redness that gets worse
- Seeing halos around lights
- Tunnel vision or trouble seeing to the side
- Nausea or headaches with eye pain
These could mean rising eye pressure or an infection. Don’t wait. Even if you’re not sure, it’s better to get checked.
Stopping Steroid Drops Safely
Never quit cold turkey. Stopping suddenly can cause your inflammation to come back worse than before-sometimes called rebound inflammation. Your doctor will taper your dose slowly. That might mean going from four times a day to twice a day, then once a day, then every other day over several weeks. This gives your eye time to heal without triggering a flare-up.
What If You Develop Cataracts?
If steroid use leads to cataracts, surgery is the only fix. Cataract surgery is highly successful-over 95% of patients regain clear vision. But it’s still surgery. Risks include infection (about 0.1% chance), bleeding, or posterior capsule opacification (a clouding that happens in 20% of cases within five years). That’s why avoiding cataracts in the first place is so important.
The Bottom Line
Steroid eye drops are lifesavers for serious eye inflammation. But they’re not a long-term solution. They’re like a fire extinguisher-you use them to put out a blaze, then put them back on the wall. The real danger isn’t the drops themselves-it’s using them without monitoring, without a plan, and without knowing your own risk.
If you’re on these drops, make sure you’re getting regular eye pressure checks. Ask your doctor if you’re a steroid responder. Find out what your next steps are once the inflammation clears. And never ignore new symptoms. Your vision isn’t something you can afford to gamble with.

Alec Stewart Stewart
February 4, 2026 AT 00:25Man, I was on these drops for a month after my corneal scratch. Didn’t realize how dangerous they were until my eye pressure went nuts. 😅 Glad I got checked. Docs need to spell this out way clearer.
Caleb Sutton
February 4, 2026 AT 14:23Big Pharma knows this. That’s why they push steroids-they make more money off cataract surgeries and glaucoma meds. You think your doctor cares about your vision? Nah. They’re paid by the pill.
pradnya paramita
February 5, 2026 AT 01:03It’s critical to differentiate between topical corticosteroid potency tiers. Prednisolone acetate 1% carries a significantly higher risk of IOP elevation compared to loteprednol etabonate 0.5%, which has a favorable safety profile due to its ester-based metabolism and reduced corneal penetration. Monitoring should be protocol-driven, not reactive.
Katherine Urbahn
February 6, 2026 AT 13:22It is absolutely imperative, and indeed non-negotiable, that patients adhere strictly to the prescribed regimen; furthermore, they must schedule follow-up appointments with the utmost punctuality. Failure to do so constitutes a gross negligence of one’s ocular health-and, frankly, is an irresponsible abandonment of professional medical guidance.
Jhoantan Moreira
February 8, 2026 AT 07:16Thanks for this! 🙌 So many people think "eye drops = harmless"-this is a wake-up call. I’ll be sharing this with my cousin who’s been on them for 3 months. She had no idea.
Joseph Cooksey
February 8, 2026 AT 12:29You know what’s wild? People treat these drops like they’re Visine. I’ve seen folks use leftover steroid drops from last year’s allergy flare-up like they’re buying candy. And then they show up six months later with a 40mmHg IOP and a cataract the size of a quarter. No, ma’am. No. You don’t get to play doctor with your cornea. These aren’t moisturizers-they’re chemical weapons with a prescription label.
Justin Fauth
February 9, 2026 AT 19:58So what you're saying is, if you're American and you don't have perfect health insurance, you're basically screwed? Because who the hell can afford eye pressure checks every two weeks? This system is rigged.
Meenal Khurana
February 11, 2026 AT 08:31My mom had steroid-induced glaucoma. She’s fine now, but lost 20% of her peripheral vision. Always get checked.
Joy Johnston
February 12, 2026 AT 03:35Thank you for highlighting the importance of tapering. Many patients are unaware that abrupt discontinuation can trigger rebound inflammation, which may be more severe than the initial condition. A structured, physician-supervised tapering schedule is essential to prevent this complication.
Lorena Druetta
February 12, 2026 AT 22:56You’re not alone. I was scared to stop my drops after my uveitis cleared-but my doc walked me through it step by step. You CAN get off them safely. Just don’t do it alone. 💪
Zachary French
February 13, 2026 AT 17:33So like… if u use these drops for more than 2 weeks and u dont get your eye checked, u r basically a dumbass? 😅 I mean… yeah… but like… why dont they just make a warning label bigger than a billboard???