Opioid Overdose Risk Assessment Tool
Assess Your Opioid Overdose Risk
This tool helps you determine your risk of opioid overdose based on CDC guidelines. The results are for informational purposes only and should not replace professional medical advice.
Answer these questions:
Your Risk Assessment
Risk factors identified:
When a doctor prescribes opioids for chronic pain, they’re not just giving you medicine-they’re also handing you a risk. Opioids work well for pain, but they can slow or stop your breathing, especially at higher doses or when mixed with other drugs. That’s where naloxone co-prescribing comes in. It’s not a second thought. It’s a life-saving step that’s now part of standard care for many patients on opioids.
What Is Naloxone Co-Prescribing?
Naloxone co-prescribing means giving a patient naloxone at the same time they get their opioid prescription. Naloxone isn’t a painkiller. It’s an opioid blocker. If someone overdoses, naloxone can quickly reverse the effects-often bringing them back to life within minutes. This isn’t just for people with addiction. It’s for anyone on opioids long-term, especially if they’re taking 50 morphine milligram equivalents (MME) or more per day.
Think of it like a fire extinguisher in your home. You hope you never need it, but if something goes wrong, having it nearby makes all the difference. Naloxone works the same way. It doesn’t prevent overdose. It gives you a chance to survive it.
Who Needs It?
The CDC says you should consider naloxone if you’re on opioids and any of these apply:
- You’re taking 50 MME or more per day
- You’re also on benzodiazepines (like Xanax or Valium)
- You have sleep apnea or COPD
- You’ve had a past overdose
- You use alcohol or other drugs
- You have depression, anxiety, or other mental health conditions
- You’ve recently been released from jail or prison
That last one is critical. People coming out of incarceration often lose their tolerance to opioids. If they use the same dose they did before, it can kill them. Naloxone can be the difference between life and death in those first dangerous days.
It’s not just about the dose. It’s about context. Someone on 30 MME with sleep apnea and a history of alcohol use is at higher risk than someone on 80 MME with no other health issues. Doctors are supposed to look at the whole picture-not just the number on the prescription.
How Does Naloxone Work?
Naloxone has been around since the 1960s. It works by kicking opioids off the brain’s receptors. Opioids bind to these receptors and slow your breathing. Naloxone is stronger. It grabs those receptors first, pushes the opioids out, and lets you breathe again.
The most common form today is the nasal spray-Narcan® or generic versions. You don’t need training to use it. Just tilt the head back, insert the nozzle, and press the plunger. That’s it. It works in 2-5 minutes. If the person doesn’t wake up, you give a second dose after 2-3 minutes. Emergency services still need to be called. Naloxone wears off faster than some opioids, so the overdose can come back.
There are also injectable versions, but most people and families prefer the nasal spray. It’s easier. Less scary. More likely to be used in a panic.
Why Isn’t Everyone Getting It?
Despite clear guidelines, many patients still don’t get naloxone. Why?
Some doctors don’t bring it up. A 2021 survey found that 68% of primary care doctors felt uncomfortable talking about overdose risk. They worry about offending patients. They think it implies they believe the patient will misuse their meds.
Patients, too, often react badly. One Reddit user shared that 60% of their patients refuse naloxone because they feel judged. But here’s the truth: naloxone isn’t about suspicion. It’s about safety.
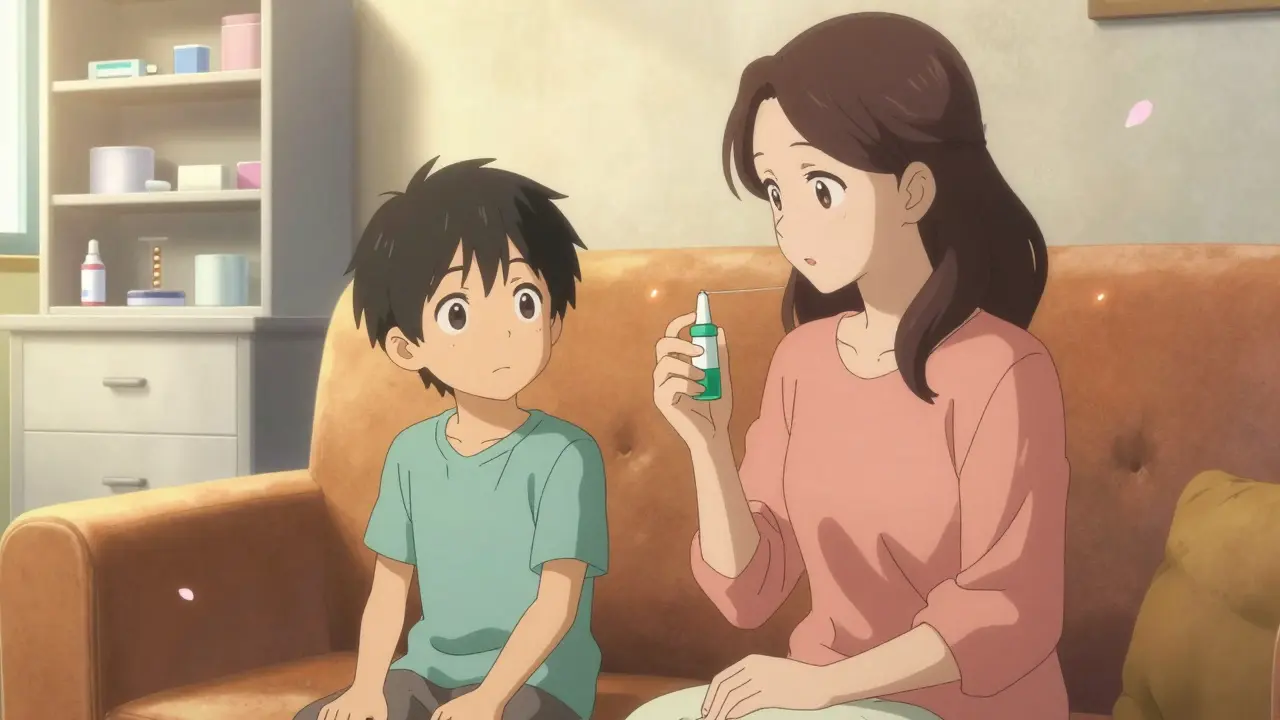
Take Sarah Johnson’s story. She was angry when her doctor prescribed naloxone with her oxycodone. But when her 16-year-old son found her pills and took them accidentally, the nasal spray saved his life. She later said, “I’m not angry anymore. I’m grateful.”
Stigma is real. But so is the risk.
Cost and Access
Generic naloxone nasal spray costs $25-$50 without insurance. Brand-name Narcan® can run $130-$150. But since the SUPPORT Act passed in 2018, most insurers cover it with little or no copay. Medicare and Medicaid must cover it. Many pharmacies now stock it for free under standing orders-no prescription needed.
Still, access isn’t equal. Urban pharmacies stock naloxone 85% of the time. Rural pharmacies? Only 42%. That’s a dangerous gap. If you live outside a city, you might have to drive farther or ask your doctor to mail it.
Since 2022, generic versions have flooded the market. Prices dropped. Availability rose. The FDA approved its first generic nasal spray in April 2023. That’s good news. More people can get it.
What’s Changing Now?
The CDC updated its guidelines in August 2023. Now, they say: if you’ve had a non-fatal overdose in the past year, you should get naloxone-even if you’re on a low dose. That’s a big shift. It means the focus isn’t just on dose anymore. It’s on history.
States are changing too. In New York, every patient getting an opioid prescription must be offered naloxone. In California, it’s required if you’re on more than 90 MME/day. Twenty-four states now have laws requiring it in some form.
And the federal government is investing. The Biden administration’s 2024 budget includes $500 million specifically for naloxone distribution. The NIH is funding research into long-acting naloxone-something that could last for weeks instead of hours. That could be a game-changer for people in recovery.
What Happens When It’s Used?
A 2019 study in the Annals of Internal Medicine looked at 1,985 patients. Those who got naloxone with their opioid prescription had 47% fewer emergency room visits and 63% fewer hospital stays because of overdoses.
Dr. Michael Chen, a doctor in rural Kentucky, started co-prescribing in 2021. Since then, his clinic has recorded 17 overdose reversals-every one done by a family member using the nasal spray he gave them.
These aren’t statistics. These are people going home to their kids, their partners, their jobs. Naloxone doesn’t fix addiction. But it buys time. Time to get help. Time to change. Time to live.
What You Can Do
If you’re on opioids:
- Ask your doctor: “Should I have naloxone?”
- If they say no, ask why. Is it because you’re not at risk-or because they’re not trained?
- Get the nasal spray. Keep it with your pills. Or better yet, give one to a family member or friend.
- Learn the signs of overdose: slow or stopped breathing, blue lips, unresponsiveness.
- Practice using the spray. Even if you never need it, knowing how helps in a crisis.
If you’re a family member:
- Don’t assume the person on opioids doesn’t need help.
- Ask if they have naloxone. If not, help them get it.
- Keep a kit in your car, your purse, your medicine cabinet.
Naloxone isn’t a sign of failure. It’s a sign of care.
Is naloxone only for people with opioid addiction?
No. Naloxone is for anyone prescribed opioids who might be at risk of overdose-even if they take their medication exactly as directed. People with chronic pain, sleep apnea, or those taking other sedatives like benzodiazepines are at risk. Naloxone is a safety net, not a judgment.
Can I get naloxone without a prescription?
Yes, in most states. Many pharmacies offer naloxone under standing orders, meaning you can walk in and ask for it without seeing a doctor. Some states even allow pharmacies to dispense it for free. Check your local pharmacy or visit your state health department’s website.
Will naloxone work if someone overdosed on fentanyl?
Yes, but it might take more than one dose. Fentanyl is much stronger than other opioids, so sometimes two or three doses of naloxone are needed. The nasal spray is still effective. Always call 911 after giving naloxone-even if the person wakes up.
Is naloxone safe to use if I’m not sure it’s an overdose?
Yes. Naloxone is extremely safe. If the person didn’t take opioids, it won’t hurt them. If they did, it can save their life. It’s better to give it and be wrong than to wait and lose someone.
How long does naloxone last, and what happens after it wears off?
Naloxone works for 30 to 90 minutes. Many opioids last longer. So if someone overdoses on heroin or fentanyl, they can slip back into overdose after naloxone wears off. That’s why you must call 911 and stay with the person until help arrives-even if they seem fine.
Next Steps
If you’re on opioids and don’t have naloxone, talk to your doctor today. If your doctor doesn’t offer it, ask for a referral to a pharmacist who can provide it. If you’re a family member, keep a kit at home and know how to use it. Practice on a training device if one’s available.
Overdose doesn’t always happen to someone else. It can happen in your home, to someone you love. Naloxone doesn’t fix the problem-but it gives you a shot at saving a life while the real work begins.
