Metformin Dosage Calculator
This calculator helps estimate appropriate starting dose of Metformin based on kidney function and weight. Important: This is not a substitute for medical advice. Always consult your healthcare provider for personalized dosing.
Recommended Dosage
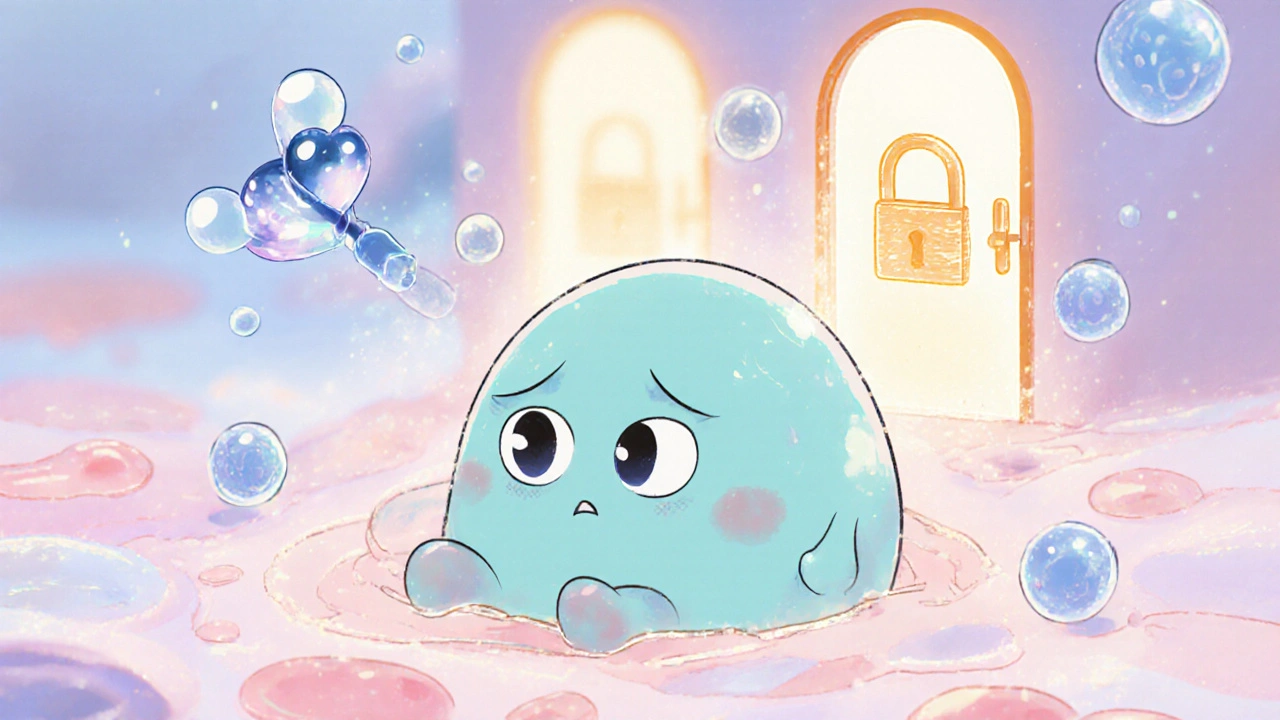
Imagine your cells ignoring the insulin signal that tells them to take in glucose - that’s insulin resistance, a silent driver behind weight gain, fatigue, and eventually type 2 diabetes. One of the most prescribed pills to tackle this problem is Metformin. It’s not a miracle cure, but understanding how it works can empower you to make better health choices.
What Is Insulin Resistance?
Insulin resistance occurs when the body’s cells-especially muscle, fat, and liver-become less responsive to insulin, the hormone that opens the door for glucose to enter cells for energy. Instead of being used, glucose stays in the bloodstream, raising blood sugar levels. Over time, the pancreas tries to compensate by producing more insulin, leading to a vicious cycle.
Insulin resistance is a metabolic condition in which normal concentrations of insulin produce a suboptimal cellular response, causing elevated blood glucose and increased insulin secretion. Common contributors include excess abdominal fat, sedentary lifestyle, chronic inflammation, and genetics.
Conditions linked to insulin resistance include prediabetes, type 2 diabetes, polycystic ovary syndrome (PCOS), and metabolic syndrome. Even if you haven’t been diagnosed with any of those, the underlying resistance can silently harm your heart, kidneys, and brain.
How Metformin Works - The Core Mechanisms
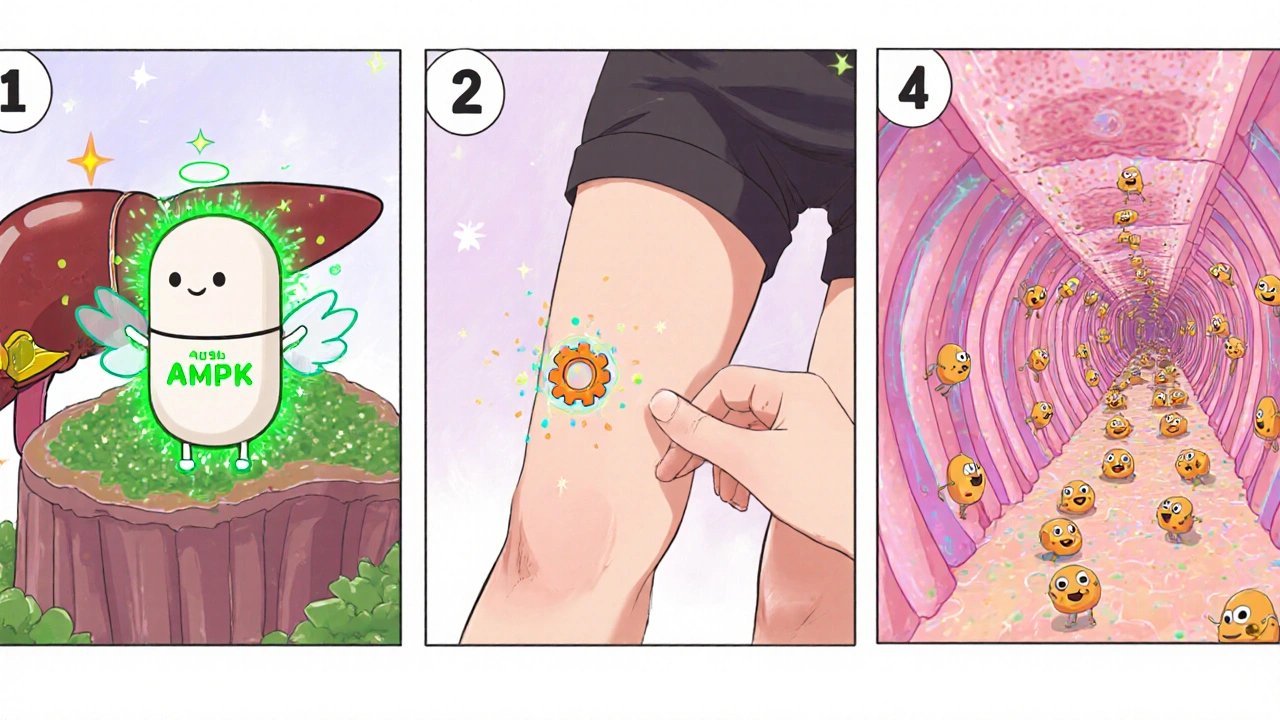
The first thing to know is that Metformin isn’t a hormone or a secret‑secretagogue; it’s a biguanide that primarily targets the liver. Its actions can be grouped into three interconnected pathways:
- Reducing hepatic glucose production - Metformin activates an enzyme called AMP‑activated protein kinase (AMPK). When AMPK is switched on, the liver’s “glucose‑making” machinery (gluconeogenesis) slows down.
- Improving peripheral glucose uptake - By boosting AMPK in muscle and fat, Metformin helps cells absorb more glucose without needing extra insulin.
- Modulating the gut - The drug alters the intestinal microbiome and reduces glucose absorption from the gut, adding a modest but measurable effect on blood sugar.
AMPK is an energy‑sensing enzyme that, when activated, promotes catabolic pathways (like glucose uptake) and inhibits anabolic pathways (like glucose production). Metformin’s ability to turn on AMPK makes it a metabolic “reset button,” nudging the body toward a leaner, more insulin‑sensitive state.
Unlike insulin, Metformin doesn’t force cells to take up glucose; instead, it lowers the amount of glucose the liver releases and makes the peripheral tissues a bit more receptive to the insulin that is already present.
Beyond Blood Sugar - Extra Health Benefits
Doctors love Metformin because the evidence shows benefits that stretch past glucose control:
- Weight management - Many users experience modest weight loss (1-3 kg) as a by‑product of better insulin signaling and reduced appetite.
- Cardiovascular protection - Large trials (e.g., UKPDS) found lower rates of heart attacks and strokes among Metformin users compared with other diabetes medications.
- Potential anti‑aging effects - Laboratory studies suggest AMPK activation may improve cellular repair pathways, a theory that’s now being tested in human trials.
- Gut microbiome balance - Metformin encourages growth of beneficial bacteria like Akkermansia muciniphila, which itself is linked to improved insulin sensitivity.
Gut microbiome refers to the trillions of microorganisms residing in the gastrointestinal tract that influence digestion, immunity, and metabolic health. Shifts in these microbes can partly explain why some people feel better after starting Metformin.
Who Might Benefit From Metformin?
Metformin isn’t a one‑size‑fits‑all solution, but it’s considered first‑line for several groups:
- People with type 2 diabetes - It’s the most prescribed oral medication worldwide.
- Individuals with prediabetes and high insulin levels - Doctors may prescribe it to delay progression to full diabetes.
- Women with PCOS - By improving insulin sensitivity, Metformin can help regulate menstrual cycles and reduce androgen levels.
- Those with metabolic syndrome - When combined with diet and exercise, it can help lower waist circumference and triglycerides.
Before starting, a healthcare provider will check kidney function (eGFR ≥ 45 mL/min/1.73 m²) and screen for liver disease. It’s not recommended for pregnant women, people with severe heart failure, or anyone with a history of lactic acidosis.
Metformin vs. Other Insulin‑Sensitizing Options
While Metformin is the go‑to drug, other therapies exist. Below is a quick side‑by‑side look at the most common alternatives.
| Feature | Metformin | Pioglitazone | GLP‑1 Agonist (e.g., liraglutide) | Lifestyle (diet + exercise) |
|---|---|---|---|---|
| Primary Mechanism | AMPK activation + ↓ hepatic glucose output | PPARγ activation → ↑ insulin sensitivity in fat cells | Enhances glucose‑dependent insulin secretion, slows gastric emptying | Weight loss, improved muscle insulin signaling |
| Typical Dose | 500 mg - 2,000 mg daily | 15 - 45 mg daily | 0.6 - 1.8 mg daily (injectable) | Varies - calorie‑controlled diet, ≥150 min/week activity |
| Weight Impact | Modest loss or neutral | Neutral or slight gain | Significant loss (2-5 kg) | Potentially >5 kg loss |
| Cardiovascular Benefit | Reduced MI/stroke risk in major trials | Mixed data - may increase heart‑failure risk | Strong reduction in major adverse cardiac events | Depends on adherence; can improve lipid profile |
| Common Side Effects | GI upset, B12 deficiency | Weight gain, edema, risk of fractures | Nausea, vomiting, possible pancreatitis | Hunger, fatigue during transition |
| Contraindications | Severe renal impairment, lactic acidosis risk | Heart failure, bladder cancer history | Personal/family history of medullary thyroid carcinoma | None medical, but adherence is key |
In most cases, doctors start with Metformin because it’s inexpensive, widely studied, and has a solid safety profile. If additional control is needed, they may add a GLP‑1 agonist or, less often, a thiazolidinedione like Pioglitazone.
Side Effects, Safety Tips, and Monitoring
Metformin is generally well‑tolerated, but a few issues pop up for some users:
- Gastrointestinal upset - Nausea, bloating, or diarrhea are the most common. Starting with a low dose and using the extended‑release formulation can help.
- Vitamin B12 deficiency - Long‑term use can reduce B12 absorption. Check levels annually after the first year.
- Lactic acidosis (rare) - A buildup of lactic acid can be fatal, but it occurs mainly when kidney function is poor or when the drug is taken in overdose.
Vitamin B12 is an essential water‑soluble vitamin needed for red blood cell formation and neurological function. If you develop tingling, fatigue, or anemia, ask your doctor for a B12 test.
Lactic acidosis describes a rare metabolic complication where lactic acid builds up faster than the body can clear it, leading to low blood pH and severe symptoms. Symptoms include rapid breathing, muscle pain, and abdominal discomfort. If any of these appear, seek emergency care.
Practical safety steps:
- Take Metformin with meals to minimize GI irritation.
- Stay hydrated - dehydration raises lactic acidosis risk.
- Schedule yearly kidney function (eGFR) and B12 labs.
- Inform your dentist and surgeon that you’re on Metformin before any procedures.
Putting It All Together - A Practical Plan
If you’ve decided to discuss Metformin with your doctor, here’s a simple roadmap:
- Get a baseline assessment - fasting glucose, HbA1c, kidney function, and B12 level.
- Start low, go slow - 500 mg once daily with dinner, then increase weekly as tolerated.
- Track your response - log blood sugar, weight, and any digestive symptoms for the first month.
- Combine with lifestyle moves - aim for 150 min of moderate exercise weekly and a diet rich in fiber, lean protein, and healthy fats.
- Re‑evaluate every 3-6 months - adjust dose, add another agent, or consider stopping if goals are met and side effects linger.
Remember, the drug works best when your body’s overall metabolic health improves. Think of Metformin as a catalyst that helps your own insulin do its job more efficiently.
Frequently Asked Questions
Can I take Metformin if I don’t have diabetes?
Yes, some doctors prescribe it for prediabetes, PCOS, or severe insulin resistance, but it must be done under medical supervision.
How long does it take to see the benefits?
Blood sugar often improves within 1-2 weeks, while weight loss and insulin sensitivity gains become noticeable after 2-3 months of consistent use.
Is the extended‑release version better?
For many people the XR (extended‑release) pill reduces GI side effects because the drug is released slowly throughout the day.
Can Metformin cause low blood sugar?
Rarely. Metformin does not stimulate insulin release, so hypoglycemia usually only occurs when combined with other glucose‑lowering meds or skipped meals.
Should I stop Metformin before surgery?
Many surgeons advise holding Metformin 24‑48 hours before major procedures to reduce lactic acidosis risk in case of dehydration.
Bottom Line
Metformin is a well‑studied, affordable tool that tackles insulin resistance at its source. When paired with a balanced diet, regular movement, and routine monitoring, it can lower blood sugar, aid modest weight loss, and protect the heart. Talk to a healthcare professional to see if it fits your personal health roadmap.
Kristin Violette
October 23, 2025 AT 23:24Insulin resistance epitomizes a pathological desensitization of the insulin receptor cascade, whereby post‑receptor signaling fidelity deteriorates. At the molecular tier, serine phosphorylation of IRS‑1 impedes PI3K activation, curtailing GLUT‑4 translocation to the sarcolemma. Concomitantly, hepatic gluconeogenesis persists unabated due to diminished AMPK‑mediated inhibition of the transcriptional co‑activator CREB. Metformin, a hydrophilic biguanide, circumvents these aberrations by potentiating AMPK, which orchestrates a catabolic shift. Activation of AMPK phosphorylates ACC, attenuating malonyl‑CoA synthesis and thereby enhancing fatty acid oxidation. The downstream effect includes a rebalancing of the NAD⁺/NADH ratio, fostering mitochondrial efficiency. Clinically, this manifests as a modest reduction in fasting plasma glucose, typically in the range of 0.5–1.0 mmol/L. Moreover, the drug's influence on the intestinal microbiota-particularly enrichment of Akkermansia muciniphila-exerts secondary insulin‑sensitizing effects. Patients frequently report ameliorated satiety signals, which can be attributed to altered short‑chain fatty acid production. From a cardiovascular perspective, the UKPDS demonstrated a statistically significant decrement in macrovascular events among metformin cohorts. The drug’s safety profile is reinforced by its negligible risk of hypoglycemia when administered as monotherapy. Nevertheless, clinicians must vigilantly monitor renal function, as eGFR thresholds below 45 mL/min/1.73 m² contraindicate usage. Long‑term therapy may precipitate subclinical vitamin B12 malabsorption, warranting periodic hematologic assessment. In the context of polycystic ovary syndrome, enhanced insulin sensitivity translates to reduced ovarian androgen synthesis. Lifestyle optimization-dietary modulation, structured aerobic exercise, and sleep hygiene-synergizes with metformin’s pharmacodynamics. Thus, metformin should be envisioned as a metabolic catalyst that amplifies endogenous insulin efficacy rather than a substitute for holistic health practices.
Diane Larson
October 30, 2025 AT 21:04Metformin truly transformed my PCOS management, especially when paired with consistent movement.
Michael Kusold
November 5, 2025 AT 15:58I started metformin a month ago and the gut upset was real, i felt like my stomach was doing somersaults. The nausea faded after I split the dose and took it with dinner. Now my blood sugar numbers are slowly creeping down.
Jeremy Lysinger
November 10, 2025 AT 07:04Begin with 500 mg at dinner, then titrate up each week as tolerated. Your body will adapt and the GI side effects will subside.
Nelson De Pena
November 13, 2025 AT 18:24Your experience underscores a key therapeutic niche of metformin in reproductive endocrinology. By attenuating hyperinsulinemia, the drug reduces ovarian theca cell androgen output, which often normalizes menstrual cyclicity. Clinical trials have documented a 30‑40 % improvement in ovulatory rates among women with PCOS on metformin monotherapy. Importantly, these benefits persist when lifestyle interventions are concurrently implemented. Thus, your anecdotal outcome aligns with the broader evidence base.
Wilson Roberto
November 16, 2025 AT 01:58The mechanistic cascade you described reflects a broader principle: pharmacologic agents can modulate endocrine feedback loops without overriding physiological autonomy. Metformin's subtle amplification of insulin signaling respects the body's intrinsic homeostatic set points. When patients internalize this nuance, adherence improves because the medication is perceived as a partner rather than a crutch. Moreover, the gut microbiome alterations you mentioned illustrate the interconnectedness of metabolic and immune networks. Recognizing these layers transforms a simple prescription into a conduit for systemic resilience.
Narasimha Murthy
November 19, 2025 AT 13:18While metformin enjoys a venerable reputation, its pharmacological profile warrants a measured appraisal. The drug’s modest efficacy in glycemic reduction is often overstated relative to emerging sodium‑glucose cotransporter‑2 inhibitors. Furthermore, gastrointestinal intolerance leads to discontinuation in a non‑trivial proportion of patients, diminishing real‑world effectiveness. The reliance on surrogate endpoints in many landmark trials leaves uncertainties about long‑term mortality benefits beyond cardiovascular composites. Consequently, clinicians should weigh these limitations against the drug’s cost advantage before defaulting to metformin as first‑line therapy.
Kelvin Egbuzie
November 21, 2025 AT 20:51Ah yes, because the pharmaceutical industry’s altruistic motives are crystal clear 😏. Nothing says ‘we care about you’ like a cheap biguanide that can cause lactic acidosis if you forget to hydrate. And let’s not overlook the glamorous side‑effects-vitamin B12 deficiency, anyone? So sure, keep popping metformin while the real cure sits hidden behind patents. 🙄
Katherine Collins
November 25, 2025 AT 08:11i think metformin is ok but the belly gas can be real bad 😅. still worth it if you keep track of your diet.
Taylor Nation
November 27, 2025 AT 15:44Your observation about gastrointestinal distress is valid; however, titrating the dose and utilizing the extended‑release formulation mitigates most of those symptoms. Evidence suggests that patients adhering to a low‑glycemic diet experience fewer bouts of bloating. Therefore, proactive dose management coupled with dietary vigilance maximizes therapeutic gain.
Shermaine Davis
December 1, 2025 AT 03:04I read about metformin and it sounds good. i will ask my doctor if it can help me.
tatiana anadrade paguay
December 3, 2025 AT 10:38Consulting a healthcare professional is indeed the prudent step, as they can tailor the regimen to your renal function and metabolic profile. Additionally, baseline measurements of HbA1c and vitamin B12 provide a reference point for monitoring. Integrating metformin with structured lifestyle changes often yields the most robust outcomes.
Aimee White
December 6, 2025 AT 21:58The shadowy pharmaco‑elite may have us believe metformin is the silver bullet, yet the true cure lies hidden in ancient herbal wisdom. Until we unravel that conspiracy, we remain pawns in a glucose‑driven theater.