Every year, tens of thousands of seniors end up in the hospital-not because of a fall, stroke, or heart attack-but because of a medication they were told was safe. It’s not rare. It’s not an accident. It’s a pattern. And it’s entirely preventable.
Why Seniors Are More Vulnerable to Medication Risks
As we age, our bodies change. The liver doesn’t process drugs as quickly. The kidneys filter less efficiently. Body fat increases, muscle mass declines, and brain sensitivity to certain chemicals goes up. What was a harmless dose at 45 can become dangerous at 75. The American Geriatrics Society (AGS) has spent decades tracking which medications cause the most harm in older adults. Their Beers Criteria, updated in May 2023, is the gold standard. It’s not a list of banned drugs-it’s a warning system. These are medications that, for most seniors, carry more risk than benefit. According to the CDC, nearly 40% of adults over 65 take five or more prescription drugs at once. That’s called polypharmacy. And with each added pill, the chance of a bad reaction climbs. One study found that seniors on four or more medications are twice as likely to be hospitalized for a drug-related problem.The Top 5 High-Risk Medications for Seniors
Not all risky drugs are obvious. Some are still prescribed because they’re cheap, familiar, or have been used for decades. Here are the five that need the most attention:- Zolpidem (Ambien®) - This sleep aid doesn’t just make you drowsy. It lingers in the body of older adults, causing confusion, sleepwalking, and falls. Studies show it increases hip fracture risk by 2.5 times. The AGS says it should be avoided entirely for chronic use in seniors. Safer alternatives? Trazodone or cognitive behavioral therapy for insomnia (CBT-I).
- Glyburide (Diabeta®) - A diabetes drug that can drop blood sugar too low. In seniors, this isn’t just a scare-it’s life-threatening. Glyburide causes hypoglycemia in nearly 30% of elderly patients, leading to emergency visits. Glipizide or metformin are far safer choices with lower risk of crashes.
- Diphenhydramine (Benadryl®) - Found in allergy pills, sleep aids, and even some cold medicines, this antihistamine has a high anticholinergic score. Long-term use increases dementia risk by 54%. It also causes dry mouth, constipation, blurred vision, and urinary retention. For allergies, loratadine (Claritin) or cetirizine (Zyrtec) are better. For sleep, skip it entirely.
- Promethazine (Phenergan®) - Often given for nausea or vomiting, this drug can trigger severe muscle spasms, tremors, and even seizures in older adults, especially those with Parkinson’s. One study showed it doubles seizure risk in seniors with epilepsy. Ondansetron (Zofran) is a much safer option for nausea.
- Nitrofurantoin (Macrobid®) - Used for urinary tract infections, this drug can cause deadly lung damage in seniors with reduced kidney function. The risk spikes when creatinine clearance drops below 60 mL/min. For UTIs, amoxicillin or nitroxoline are safer if kidney function is low.
What You Might Not Realize: Hidden Risks in Everyday Pills
Many seniors don’t realize their daily pills are part of the problem. Over-the-counter meds, herbal supplements, and even cough syrups can pack a dangerous punch. Take cough syrups with dextromethorphan and diphenhydramine. They’re sold as “natural sleep aids” or “cold relief.” But combined, they create a powerful anticholinergic load. One 72-year-old woman I know was taking three different products-all with diphenhydramine-and ended up in the ER with confusion and urinary retention. She didn’t know they all had the same active ingredient. Even common heartburn meds like ranitidine (Zantac) are now pulled from shelves, but older versions of H2 blockers can still interact dangerously with blood thinners. And don’t forget muscle relaxants like cyclobenzaprine. They’re often prescribed for back pain, but they cause dizziness, falls, and confusion in seniors. Physical therapy and heat packs often work better.How to Review Your Medications (Step by Step)
You don’t need to be a doctor to protect yourself or a loved one. Here’s how to do a real, effective medication review:- Collect every pill, patch, and liquid. Do a “brown bag review.” Empty everything from the medicine cabinet into a bag-prescriptions, OTCs, vitamins, supplements. Don’t leave anything out.
- Bring it to your doctor or pharmacist. Ask: “Which of these are on the Beers Criteria list?” Don’t be shy. Most doctors don’t know all 30+ high-risk drugs by heart, but pharmacists do.
- Ask about anticholinergic burden. Request the Anticholinergic Cognitive Burden (ACB) score for each drug. Add them up. If the total is 3 or higher, you’re at high risk for memory problems.
- Check kidney function. Ask for your eGFR number. If it’s below 60, many drugs (like nitrofurantoin or metformin) need dose changes or replacement.
- Ask for alternatives. “Is there a safer option?” is the most powerful question you can ask. For insomnia, ask about CBT-I. For pain, ask about acetaminophen or physical therapy. For anxiety, ask about talk therapy before benzodiazepines.
- Don’t stop cold turkey. Some drugs, like benzodiazepines or antidepressants, need to be tapered slowly. Ask for a plan. Sudden withdrawal can cause seizures or rebound anxiety.
What Works Better Than High-Risk Drugs
The good news? There are safer, often more effective options for almost every high-risk medication.- For sleep: Skip zolpidem. Try melatonin (3 mg at bedtime), CBT-I, or trazodone (50 mg). CBT-I has been shown to work better than pills long-term.
- For diabetes: Skip glyburide. Use metformin, GLP-1 agonists like semaglutide, or glipizide. These don’t cause dangerous low blood sugar.
- For allergies: Skip diphenhydramine. Use loratadine, cetirizine, or fexofenadine. They don’t cross the blood-brain barrier.
- For nausea: Skip promethazine. Use ondansetron. It’s not sedating and doesn’t cause muscle rigidity.
- For anxiety or agitation: Skip benzodiazepines like lorazepam. Try SSRIs, cognitive behavioral therapy, or environmental changes-like reducing noise or improving lighting.
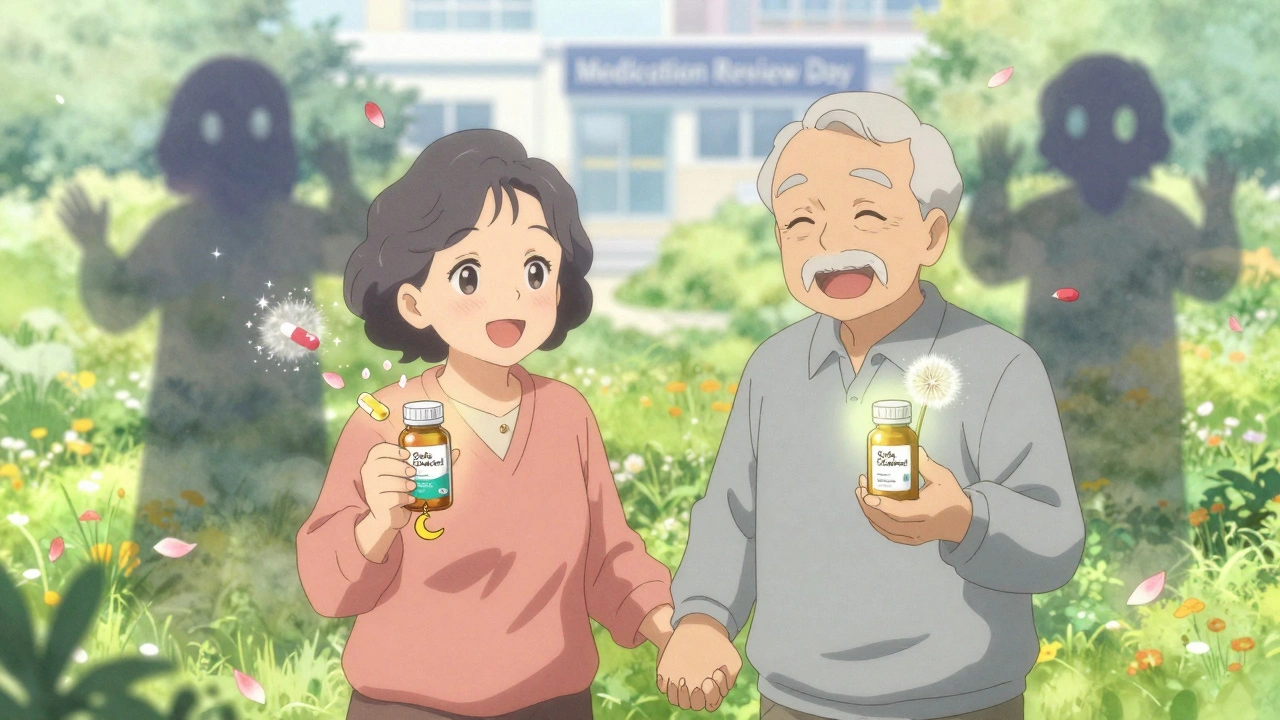
What Health Systems Are Doing About It
It’s not just up to you. The system is slowly changing. In 2024, Medicare Advantage plans started tying 5% of their quality bonuses to reducing high-risk prescriptions. Pharmacies now use real-time alerts when a doctor tries to prescribe zolpidem or glyburide to a senior. Electronic health records like Epic and Cerner now flag Beers Criteria drugs automatically. Pharmacists are now part of the care team in many clinics. One study showed that when a clinical pharmacist reviews a senior’s meds, high-risk drug use drops by 35% in six months. But these tools only work if you’re aware of them. If your doctor doesn’t mention medication safety, ask. If your pharmacist doesn’t review your list, request it.What to Do If You’re Already on a High-Risk Drug
If you’re taking one of these drugs right now, don’t panic. But don’t ignore it either. Start by writing down:- Why you were prescribed it
- How long you’ve been taking it
- Any side effects you’ve noticed (dizziness, confusion, constipation, falls)
- Whether you’ve ever been told there’s a safer option
Final Thought: Medication Review Isn’t a One-Time Task
Your body changes. Your health changes. Your meds should change too. A medication review isn’t something you do once a year. It’s something you do every time you see a new doctor, start a new treatment, or feel off. If you’re on five or more drugs, make it a habit-every six months. The goal isn’t to cut pills. It’s to keep you safe, sharp, and strong. You’ve earned that.What are the most dangerous medications for seniors?
The most dangerous medications for seniors include zolpidem (for sleep), glyburide (for diabetes), diphenhydramine (in allergy and sleep meds), promethazine (for nausea), and nitrofurantoin (for UTIs). These drugs increase risks of falls, confusion, low blood sugar, lung damage, and dementia. The American Geriatrics Society’s Beers Criteria lists 30+ such medications, updated in 2023.
How do I know if a medication is high-risk for my age?
Ask your pharmacist or doctor to check your meds against the AGS Beers Criteria. You can also look up each drug on the Anticholinergic Cognitive Burden (ACB) scale-scores above 1 are risky, and above 3 are very high. If you’re over 65 and taking more than five drugs, assume at least one might be high-risk and get it reviewed.
Can I stop taking a high-risk medication on my own?
No. Stopping some medications suddenly-like benzodiazepines, antidepressants, or steroids-can cause seizures, rebound anxiety, or dangerous withdrawal. Always talk to your doctor first. They can help you taper safely, often over 4-6 weeks, and replace it with a safer option.
Are over-the-counter drugs safe for seniors?
Many are not. OTC sleep aids, allergy pills, and cold medicines often contain diphenhydramine or other anticholinergics. These can cause confusion, dry mouth, constipation, and memory problems. Always read labels. Look for non-drowsy versions like loratadine instead of Benadryl, or acetaminophen instead of combination pain relievers.
What should I ask my doctor during a medication review?
Ask: 1) Is this drug on the Beers Criteria list? 2) What’s the anticholinergic burden? 3) Is there a safer alternative? 4) Can we reduce the dose or stop it? 5) How will we know if it’s working? Write these down. Bring a list of all your meds. Most doctors welcome this level of engagement.
How often should seniors review their medications?
At least once a year. But if you’re on five or more medications, or if you’ve recently seen a new doctor, changed hospitals, or started a new treatment, do a review every six months. Your body changes-and your meds should too.

John Fred
December 13, 2025 AT 06:49OMG this is LIFE-SAVING info!!! 🚨 I had no idea Benadryl was basically a dementia accelerator for seniors. My grandma’s been on it for years for ‘sleep’-time to swap her to loratadine ASAP. Also, CBT-I? That’s a thing?? I’m printing this out and mailing it to my entire family. 🙌 #BeersCriteriaIsTheNewGospel
Harriet Wollaston
December 13, 2025 AT 11:48This made me cry-literally. My mom’s on five meds, and I never asked if any were risky. I just assumed doctors knew best. Turns out, they’re overloaded too. I’m scheduling a brown bag review this week. Thank you for writing this like you were talking to your own family. You didn’t just inform-you healed something.
Lauren Scrima
December 14, 2025 AT 16:34Wow. Just… wow. So, what you’re saying is… doctors are still prescribing Ambien like it’s candy?? And we’re surprised seniors are falling?!!?? 🤦♀️ Also, ‘nitrofurantoin causes lung damage’-and yet, it’s still on every UTI script?? Someone’s getting paid to keep this going.
Himmat Singh
December 16, 2025 AT 01:33It is, with due respect, an oversimplification to attribute polypharmacy-related morbidity solely to pharmacological factors. The socio-economic determinants of healthcare access, coupled with fragmented care delivery systems, constitute a more profound structural challenge. One cannot reduce systemic failure to a mere list of drugs.
Webster Bull
December 16, 2025 AT 11:51STOP. Just… stop. I’ve been telling my dad for years to ditch his diphenhydramine. He said ‘but it helps me sleep!’ Bro. It’s making him forget his own name. Time to try melatonin. 3mg. Done. No drama. No pills. Just sleep. 🙏
nithin Kuntumadugu
December 17, 2025 AT 02:08THIS IS A PHARMA CONSPIRACY. 😈 They don’t want you to know that CBT-I is FREE and works BETTER than Ambien. Why? Because pills = profit. And guess who owns the patents? Big Pharma. They’re poisoning grandma to keep their stock up. 🤫 Look into the ‘Beers Criteria’-it’s been buried for 20 years. The FDA knows. They just don’t care.
Hamza Laassili
December 18, 2025 AT 23:42Y’all need to stop letting these ‘experts’ tell you what to do. We used to take these meds in the 80s and we were FINE. Now it’s ‘oh no, seniors can’t take anything!’ This is just woke medicine. They’re trying to scare us into taking ‘safer’ drugs that cost $300 a month. My uncle’s 82 and still takes Benadryl-he sleeps like a baby. Who are you to say he’s wrong?
Casey Mellish
December 20, 2025 AT 22:16Brilliantly articulated. The Beers Criteria isn’t just a list-it’s a cultural shift in geriatric care. I’ve trained pharmacists in Australia using this exact framework. The real win? When patients bring the list themselves. That’s when change happens. Keep pushing. We’re all better off when seniors aren’t medicated into oblivion.
Tyrone Marshall
December 21, 2025 AT 18:55There’s a quiet revolution happening here. It’s not about taking pills away-it’s about giving people back their dignity. Sleep without confusion. Pain without dizziness. Peace without dependency. This isn’t just medicine. It’s respect. And honestly? If your mom or dad is on 5+ meds, you owe it to them to ask: ‘Is this helping me… or just keeping the machine running?’
Emily Haworth
December 21, 2025 AT 20:13Wait… so you’re saying the government knows this but doesn’t stop it?? 😳 I think my doctor’s in on it. I found a hidden file on his computer labeled ‘Seniors_Meds_Profit_2023’. I’m calling the FBI. And also-did you know that the FDA gets funding from drug companies?? I’m not paranoid. I’m PREPARED.
Yatendra S
December 22, 2025 AT 09:58Existentially, isn’t it ironic? We prolong life with pharmaceuticals… only to erode the very consciousness that makes life meaningful. The body survives. But the soul? The mind? That’s the real casualty. We treat symptoms, not essence. And in doing so… we become the architects of our own quiet erasure.
kevin moranga
December 22, 2025 AT 19:23Let me tell you what happened to my aunt. She was on glyburide for 8 years. One morning, she passed out in the kitchen. Paramedics said her blood sugar was 38. She spent three days in ICU. Now she’s on metformin. No more scares. No more ER trips. She’s gardening again. 🌷 The point? You don’t have to accept ‘this is just how it is.’ You can ask for better. And you deserve better. Seriously-go talk to your pharmacist today. They’re the real heroes here. And if you’re on 5+ meds? You’re already one step away from disaster. Don’t wait for the fall. Do the review. Now. I’m not saying it’s easy. But it’s worth it. Your brain, your balance, your freedom… they’re all on the line.
Bruno Janssen
December 24, 2025 AT 04:11I read this… and I just sat there. My dad’s on all five of these. I didn’t know. I thought he was just ‘getting old.’ Now I feel like I failed him. I’m going to call his doctor tomorrow. I just… needed to say that out loud.