Itch Triggers Calculator
Your Diet Assessment
Select foods you consume regularly. This tool analyzes your diet against itch-triggering foods.
Your Itch Assessment
Start by adding more anti-inflammatory foods and reducing histamine triggers.
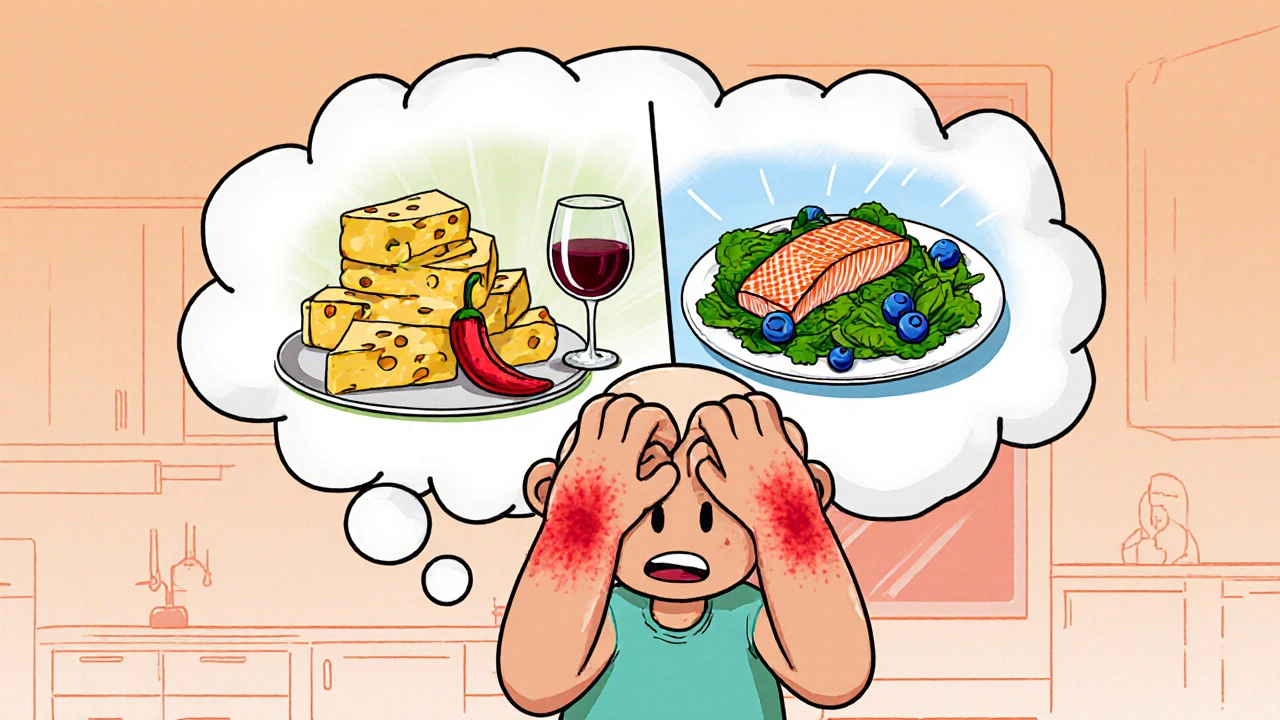
When Itching is an irritating sensation that triggers a strong urge to scratch, often caused by allergies, eczema, or dry skin, many people think only creams or medicines can help. In reality, what you eat can calm or worsen that itch. diet and itching are tightly linked, and tweaking your meals can bring real relief without a pharmacy visit.
Diet the regular selection of foods and drinks you consume supplies the nutrients that keep skin cells healthy, controls inflammation, and regulates the chemicals that trigger itch signals. Below, we break down how food influences skin, which ingredients act like a soothing balm, and which ones behave like a hidden fire‑starter.
Why What You Eat Matters for Itching
Skin is the body’s largest organ, and it relies on a steady stream of vitamins, minerals, and healthy fats to stay resilient. When the diet lacks these building blocks, the skin barrier weakens, becoming more permeable to irritants and allergens.
Two biochemical pathways are especially important:
- Inflammation control: Certain foods raise the body’s inflammatory markers (like C‑reactive protein). Higher inflammation fuels conditions such as eczema or psoriasis, each of which features chronic itch.
- Histamine regulation: Histamine is a compound released by immune cells that makes blood vessels leaky and nerves more sensitive. Some foods are high in histamine or trigger its release, turning a mild itch into a relentless burn.
By choosing anti‑inflammatory, low‑histamine foods, you can lower the baseline itch level and give topical treatments a better chance to work.
Top Anti‑Itch Foods to Add to Your Plate
These ingredients supply skin‑protecting nutrients and keep histamine in check.
- Omega‑3 fatty acids essential fats found in fatty fish, flaxseed, and walnuts that reduce inflammation. Aim for two servings of salmon or a tablespoon of ground flaxseed each day.
- Probiotics beneficial bacteria that support gut health and can calm skin irritation. Include yogurt, kefir, or fermented vegetables like kimchi.
- Vitamin D helps regulate the immune response and strengthens the skin barrier. Sun‑exposed mushrooms, fortified milk, and safe sunlight are reliable sources.
- Quercetin a flavonoid with natural antihistamine properties. Found in apples, berries, and onions; a daily handful of berries adds a sweet anti‑itch boost.
- Zinc supports skin repair and reduces inflammation. Pumpkin seeds and lean beef are zinc-rich choices.
- Bright green vegetables (spinach, kale) packed with antioxidants that neutralize free radicals that can aggravate itch.
Common Itch‑Triggering Foods to Limit or Eliminate
These items are notorious for raising histamine levels or sparking inflammation.
- Gluten a protein in wheat, barley, and rye that can provoke immune reactions in sensitive individuals. If you notice flare‑ups after bread or pasta, try a gluten‑free alternative.
- Dairy particularly cheese and whole milk, which can be high in histamine. Opt for lactose‑free milk or fortified plant milks.
- Processed meats (salami, bacon) that contain nitrates and high histamine.
- Alcohol, especially red wine, which releases histamine and dilates blood vessels, intensifying itch.
- Spicy foods (chili, hot sauces) that stimulate nerve endings and can worsen itch sensations.
- Excessive sugar, which fuels inflammation and can disrupt gut bacteria balance.

Quick Comparison: Foods to Eat vs. Foods to Avoid
| Category | Examples | Why It Helps / Hurts |
|---|---|---|
| Eat | Salmon, flaxseed, walnuts, yogurt, berries, leafy greens | Provides omega‑3s, probiotics, antioxidants, and low histamine - all calm inflammation. |
| Avoid | Wheat bread, cheese, processed meats, red wine, chili, sugary snacks | High in histamine or inflammatory compounds that exacerbate skin irritation. |
Sample 7‑Day Itch‑Friendly Meal Plan
Use this as a template; adjust portions to match your calorie needs.
- Day 1: Breakfast - Greek yogurt with chia seeds and blueberries; Lunch - Quinoa salad with spinach, avocado, and grilled salmon; Dinner - Stir‑fried bokchoy with ginger and tofu.
- Day 2: Breakfast - Oatmeal made with almond milk, topped with sliced apple and cinnamon; Lunch - Lentil soup with carrots and kale; Dinner - Baked cod with lemon, served with roasted sweet potatoes.
- Day 3: Breakfast - Smoothie (banana, spinach, flaxseed, oat milk); Lunch - Turkey lettuce wraps with cucumber and hummus; Dinner - Grilled shrimp over brown rice and steamed broccoli.
- Day 4: Breakfast - Scrambled eggs with mushrooms and a side of sliced orange; Lunch - Chickpea salad with olives, tomatoes, and olive oil; Dinner - Beef stir‑fry with bell peppers (avoid hot sauce).
- Day 5: Breakfast - Cottage cheese (lactose‑free) with pineapple chunks; Lunch - Sardine salad on gluten‑free toast; Dinner - Roasted chicken thighs with rosemary, served with quinoa.
- Day 6: Breakfast - Buckwheat pancakes topped with fresh berries; Lunch - Miso soup with seaweed and tofu; Dinner - Grilled salmon with a side of asparagus.
- Day 7: Breakfast - Chia pudding with coconut milk and mango; Lunch - Mixed bean salad with cilantro and lime; Dinner - Baked trout with cauliflower mash.
Notice the repeated inclusion of omega‑3 fish, leafy greens, and probiotic‑rich items. Each meal also avoids the trigger list.
Tracking Your Progress
Keeping a simple food‑itch diary helps pinpoint personal culprits. Record:
- What you ate (including sauces and drinks).
- Any itch flare‑ups (time, severity, location).
- Other factors (stress level, weather, skincare products).
After a week, look for patterns. If certain foods consistently precede a flare‑up, try eliminating them for another two weeks and see if symptoms improve.
Common Pitfalls and How to Avoid Them
- Thinking “healthy” means “safe”: A salad topped with aged cheese can still spike histamine. Always check the ingredient list.
- Skipping meals: Going too long without food can increase cortisol, which may heighten itch perception.
- Relying on supplements alone: Whole foods deliver synergistic nutrients that powders can’t fully replicate.
- Not staying hydrated: Dehydration dries out skin, making it easier to itch. Aim for at least eight glasses of water daily.
When to Seek Professional Help
If dietary changes reduce itch but it persists, or if you notice severe rash, swelling, or difficulty breathing, consult a dermatologist or allergist. They can test for specific food allergies, prescribe targeted topical treatments, or suggest prescription‑level dietary plans.
Frequently Asked Questions
Can a gluten‑free diet help with eczema?
For people with a gluten sensitivity, removing wheat, barley, and rye often lessens skin inflammation, which can lead to fewer itch episodes. However, if you test negative for celiac disease or gluten intolerance, a strict gluten‑free diet may offer little benefit.
Do probiotic supplements work better than food sources?
Whole‑food sources like yogurt, kefir, and fermented veggies provide a wider variety of strains and also contain fiber that feeds good gut bacteria. Supplements can be useful if you can’t tolerate dairy, but they should complement, not replace, probiotic‑rich foods.
Is fish the only source of omega‑3 for an itch‑friendly diet?
No. Flaxseed, chia seeds, walnuts, and algae‑based supplements also deliver omega‑3s, especially the plant‑based ALA form, which the body can convert to EPA/DHA needed for anti‑inflammatory effects.
How quickly can I expect to feel less itchy after changing my diet?
Results vary, but many people notice a reduction in itch intensity within two to three weeks as skin barrier function improves and inflammation drops.
Should I avoid all dairy, even low‑fat options?
If you’re sensitive to histamine, even low‑fat cheeses can trigger itch. Try a dairy‑free week; if symptoms improve, consider limiting dairy or switching to fortified plant milks.
Sumit(Sirin) Vadaviya
October 16, 2025 AT 12:00Thank you for outlining the connection between diet and itchiness; the explanation of histamine pathways is particularly clear 😊. Incorporating omega‑3 rich foods such as salmon and walnuts can indeed help to modulate inflammation, while reducing high‑histamine items like aged cheeses may lower flare‑ups. Maintaining a balanced intake of probiotics and vitamin D further supports skin barrier function. Overall, the dietary guidelines presented are practical and evidence‑based.
lindsey tran
October 17, 2025 AT 11:49OMG this is like a total game‑changer for my eczema!!! I totally definetly didn't realize cheddar could be such a sneaky itch‑trigger 😱. Switching to almond milk and loading up on berries made my skin feel sooo calmer, like the storm finally passed. Keep the tips comin', I'm vibing with this whole anti‑itch diet thing!!!
Krishna Sirdar
October 18, 2025 AT 11:38Reading through the list, I’m reminded how our bodies are like ecosystems, where each bite sends a ripple through the skin’s shield. When we give it omega‑3s, probiotics, and vibrant greens, we feed the good microbes and calm the fire of inflammation. Conversely, processed meats and excess sugar act like tiny saboteurs, nudging the immune system toward histamine release. It’s helpful to see the science broken down into everyday meals, because that makes the changes feel doable rather than overwhelming. By tracking what we eat and how our skin reacts, we can discover personal patterns that guide us toward lasting relief.
becca skyy
October 19, 2025 AT 11:27Totally agree, it’s all about the little choices we make every day. Swapping out a bag of chips for a handful of pumpkin seeds is a simple swap that can make a difference. Plus, adding a side of spinach to dinner is easy and packs a punch of antioxidants.
Theo Roussel
October 20, 2025 AT 11:16The mechanistic underpinnings articulated herein align with current immunometabolic literature, wherein eicosapentaenoic acid (EPA) serves as a precursor for resolvins that attenuate NF‑κB mediated cytokine cascades. Moreover, the catabolic degradation of histamine via diamine oxidase is modulated by dietary cofactors such as copper and vitamin C, underscoring the necessity of a micronutrient‑rich regimen. From a dermatological perspective, the integration of prebiotic fibers can recalibrate dysbiosis, thereby fortifying the stratum corneum’s permeability barrier.
Erick Masese
October 21, 2025 AT 11:05Honestly, the article cuts through the hype and gets straight to what matters: eat the good stuff, ditch the bad. It’s a straightforward prescription that anyone can follow without needing a PhD. The tone is welcoming and the science is sound, which makes the advice feel both credible and accessible.
tierra hopkins
October 22, 2025 AT 10:54Great rundown! I especially like the emphasis on staying hydrated-so many people overlook that simple step. If we all commit to swapping one sugary snack for a fruit serving each day, the cumulative impact on skin health could be huge. Let’s make these tweaks a habit and watch the itch recede.
Ryan Walsh
October 23, 2025 AT 10:43Exactly, habit stacking works wonders. I start my mornings with a kefir smoothie, then I’ve never looked back. It’s a low‑effort addition that keeps the gut happy and the skin calm.
Kiersten Denton
October 24, 2025 AT 10:32This is super useful.
Karl Norton
October 25, 2025 AT 10:21While the list is comprehensive, it glosses over the fact that many of these “anti‑itch” foods are expensive and inaccessible for low‑income families, which makes the advice feel out of touch.
Ashley Leonard
October 26, 2025 AT 09:09I love how the article breaks down each food group with clear reasons. It’s easy to copy‑paste the suggestions into a grocery list, which makes implementation a breeze.
Ramanathan Valliyappa
October 27, 2025 AT 08:58The recommendations are logical; however, the article lacks quantitative data on the magnitude of itch reduction per food item, which would strengthen the argument.
lucy kindseth
October 28, 2025 AT 08:47When tackling chronic itch, it’s essential to view nutrition as a foundational pillar rather than an afterthought. First, omega‑3 fatty acids such as EPA and DHA, found in fatty fish and algae, actively dampen the production of pro‑inflammatory eicosanoids that sensitize nerve endings. Second, the gut‑skin axis plays a pivotal role; a diverse microbiome nurtured by fermented foods like kefir, sauerkraut, and probiotic‑rich yogurt can reduce systemic inflammation that often manifests as skin irritation. Third, vitamin D not only supports immune regulation but also fortifies the epidermal barrier, making it less permeable to allergens. Fourth, antioxidants abundant in leafy greens, berries, and cruciferous vegetables scavenge free radicals that otherwise degrade collagen and exacerbate itching. Fifth, zinc contributes to cellular repair mechanisms and can moderate histamine release, especially when sourced from pumpkin seeds or lean meats. Sixth, staying well‑hydrated ensures the skin remains supple; dehydration accelerates transepidermal water loss, which is a known itch trigger. Seventh, limiting high‑histamine foods such as aged cheeses, processed meats, and certain alcoholic beverages prevents unnecessary histamine spikes. Eighth, reducing refined sugars curbs the insulin surge that can indirectly fuel inflammatory pathways. Ninth, Gluten sensitivity, though not universal, should be evaluated because even subclinical reactions can provoke dermal inflammation. Tenth, a consistent food‑itch diary helps to personalize the plan, revealing subtle patterns that generic guidelines might miss. Eleventh, gradual implementation is key-introducing one new anti‑itch food each week allows the body to adapt without overwhelming the system. Twelfth, pairing dietary changes with gentle skin‑care routines, such as fragrance‑free moisturizers, maximizes overall relief. Thirteenth, consulting a nutritionist or dermatologist can provide targeted testing for specific allergens, ensuring that dietary modifications are both safe and effective. Finally, patience is vital; most individuals notice a measurable reduction in itch intensity within two to three weeks, but sustained benefits often require months of consistent practice. By integrating these evidence‑based strategies, you can transform your diet into a powerful ally against chronic itching.
Nymia Jones
October 29, 2025 AT 08:36While the nutritional protocol outlined appears scientifically sound, one must remain vigilant about the hidden agendas of agribusiness conglomerates that deliberately suppress low‑histamine crop varieties to maintain market dominance; thus, reliance on mainstream produce may inadvertently perpetuate the very inflammatory cycles the diet seeks to break.