Every year, millions of people in the U.S. switch from brand-name drugs to generics because they’re cheaper. But here’s the problem: many don’t realize they’re getting the same medicine. When the pill looks different-maybe it’s pink instead of white, round instead of oval-some patients think it’s a new drug. They skip doses. They panic. Some even end up in the emergency room.
This isn’t just about confusion. It’s about safety. A 2021 study in the Journal of the American Geriatrics Society found that over half of older adults taking heart medications threw away their pills when the generic version looked different. That’s not stubbornness. It’s a failure in how we communicate.
What Exactly Is Health Literacy?
Health literacy isn’t just about reading. It’s about understanding what you’re told, remembering it, and using it to make smart choices. The World Health Organization defines it as the ability to find, understand, and use health information to stay healthy. That includes knowing what your pills are for, how to take them, and whether a new-looking tablet is still the same medicine.
The U.S. Department of Health and Human Services updated this definition in 2020 to include two sides: personal health literacy (what you can do) and organizational health literacy (what doctors, pharmacies, and drug makers do to help you). Too often, the system puts the burden on the patient. If you can’t read well, don’t speak English fluently, or are overwhelmed by multiple medications, you’re at a disadvantage-and the system isn’t designed to fix that.
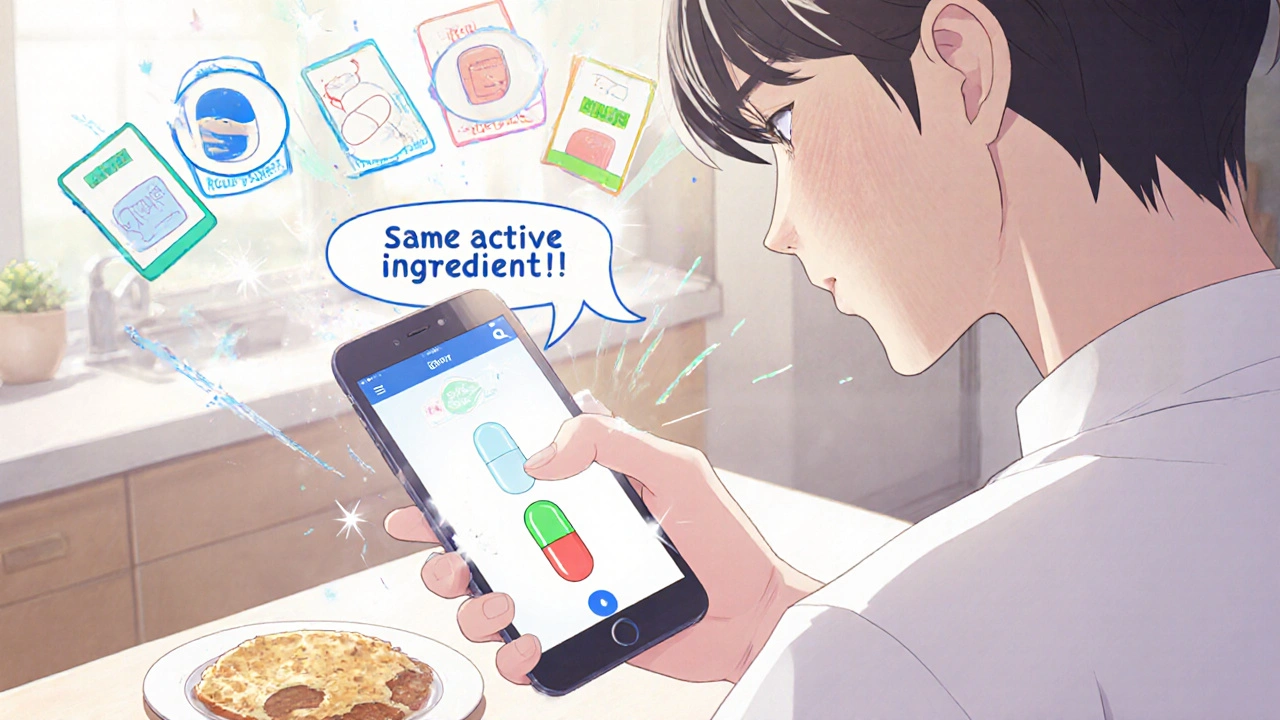
Why Generics Cause So Much Confusion
Generic drugs are chemically identical to brand-name drugs. Same active ingredient. Same dose. Same effect. But they look different. Why? Because drug companies can’t copy the exact shape, color, or logo of a brand-name pill. That’s trademark law. So a generic version of metformin might be a white oval today and a pink round tablet next month. If you’ve been taking the white one for years, you might not recognize the new one. You might think it’s something else. Or worse-you might think it’s fake.
Here’s the data: 42% of patients don’t know generics are just as effective as brand-name drugs. And it’s worse for people with low health literacy. A 2020 Kaiser Family Foundation analysis found that Medicare beneficiaries with poor reading skills were over three times more likely to refuse a generic switch-even when it was cheaper and medically identical.
Pharmacists report seeing this every week. One Reddit user who works in pharmacy wrote: “I see at least two patients weekly who refuse generics because they don’t look like what they expect.” That’s not irrational. It’s logical if you’ve never been told the truth about how generics work.
The Real Cost of Confusion
Confusion isn’t just frustrating-it’s dangerous. Between 2015 and 2020, the Institute for Safe Medication Practices recorded 1,247 medication errors caused by patients mixing up different generic versions of the same drug. That’s nearly one in five errors involving generics.
One patient with type 2 diabetes shared on PatientsLikeMe: “When my metformin changed from white oval to pink round tablets, I didn’t take it for three days thinking it was a different medication-I ended up in the ER with high blood sugar.”
And it’s not just about skipping doses. Patients sometimes take extra pills because they think the new version is weaker. Or they stop taking them altogether because they’re scared. A 2022 FDA review found that only 37% of generic drug manufacturers use plain language in their patient leaflets. That means most instructions are written in medical jargon, tiny fonts, and confusing layouts.
What’s Being Done to Fix This?
Change is happening-but slowly. Here’s what’s working:
- The “Ask Me 3” Program: Developed by the Partnership for Clear Health Communication, this simple tool trains doctors and pharmacists to ask three questions: What is my main problem? What do I need to do? Why is it important? Hospitals using this saw a 31% drop in generic-related medication errors by 2022.
- Brown Bag Reviews: Patients bring all their pills to appointments. Pharmacists or nurses sort them out and explain what each one is. A 2021 Johns Hopkins study showed this reduced medication mistakes by 44%.
- Medisafe App: This free app lets users scan their pills and get alerts when a generic changes. In a 2022 trial, it improved understanding of generics by 37% among users with low literacy.
- CDC’s Universal Precautions: Used in over 90% of Federally Qualified Health Centers, this approach treats every patient as if they might have low health literacy. It uses pictures, simple words, and repeat-backs. One evaluation showed a 52% drop in patient confusion about generics.
Even drug makers are stepping up. The Association for Accessible Medicines runs the “Know Your Generics” campaign, reaching 12 million people a year. And in 2023, the FDA allocated $4.7 million specifically to improve how generic medications are explained to patients-double what they spent in 2019.
What’s Working in Other Countries
The U.S. isn’t alone in this problem. But some countries are ahead.
In Europe, the Falsified Medicines Directive requires standardized packaging for generics. Germany and France ran pilot programs and saw a 19% drop in medication errors. The European Medicines Agency now requires consistent appearance for generics across all member states-and early data shows a 27% reduction in errors.
Australia introduced color-coded pills by therapeutic class: all blood pressure meds are blue, all diabetes meds are green, all antidepressants are yellow. Within two years, medication errors dropped by 33%.
The WHO is now pushing for global standards. In 15 low- and middle-income countries, pilot programs using visual consistency (same color, same shape for the same drug) improved correct medication use by 41%.

What You Can Do Right Now
If you or someone you care about takes generics, here’s what to do:
- Ask the pharmacist: “Is this the same medicine I’ve been taking, just a different look?” Don’t assume it’s the same. Ask.
- Keep a list: Write down the name (brand and generic), color, shape, and what it’s for. Keep it in your wallet or phone.
- Use the Medisafe app: It’s free. Scan your pills. It’ll tell you when a change happens and why.
- Bring all your pills to every appointment: Even if you think you know what they are. Your doctor might spot something you missed.
- Don’t stop taking a pill just because it looks different: Call your pharmacy or doctor first. Don’t guess.
The Future Is Clearer
The FDA’s 2023 draft guidance proposes a national color-coding system for generic drugs-just like Australia’s. If it’s adopted, a patient will know: “All my blood pressure pills are blue, no matter who made them.” That’s huge.
The Biden administration’s 2023 National Action Plan to Improve Health Literacy includes a goal: reduce confusion-related errors with generics by 25% by 2027. That’s ambitious. But possible-if we stop blaming patients and start fixing the system.
Health literacy isn’t about how smart you are. It’s about how clearly the system speaks to you. Generics save billions in healthcare costs. But if people don’t understand them, those savings vanish in ER visits, hospitalizations, and missed treatments. The solution isn’t more pamphlets. It’s consistent design, plain language, and accountability from drug makers, pharmacies, and doctors.
Medicine shouldn’t be a guessing game. Your pills should tell you their story-not leave you wondering.
Are generic drugs really the same as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They are required to work the same way in your body. The only differences are in color, shape, size, and inactive ingredients-which don’t affect how the drug works.
Why do generic pills look different every time I refill?
Different manufacturers make generics, and each one chooses its own color and shape to avoid trademark issues. Even if you get the same generic drug from the same pharmacy, the manufacturer might change. That’s why the pill you got last month might look different from the one you get this month-even though it’s the exact same medicine.
Can I ask my pharmacist to give me the same generic brand every time?
Yes, you can ask. Some pharmacies will try to fill your prescription with the same generic manufacturer if they have it in stock. But they aren’t required to. If consistency matters to you-especially if you have trouble recognizing pills-ask your doctor to write “Dispense as Written” on the prescription. That means the pharmacy must give you the exact brand or generic you’re used to.
What should I do if I think my generic medicine isn’t working?
Don’t assume it’s the generic. Talk to your doctor or pharmacist first. Sometimes changes in how you feel are due to other factors-diet, stress, other medications, or even the progression of your condition. But if you’ve noticed a change right after switching to a new-looking pill, mention it. Your provider can check if the dosage is right or if you’re reacting to an inactive ingredient.
Are there tools or apps that help me track my generic medications?
Yes. The Medisafe app lets you scan your pills and store their appearance, name, and instructions. It sends alerts when a refill looks different and explains why. Other apps like MyTherapy and Dosecast have similar features. These tools are especially helpful for older adults and people managing multiple medications.
How can I help an elderly relative understand their generics?
Start by making a simple visual chart: take pictures of each pill (brand and generic versions), write the name, what it’s for, and when to take it. Keep it in a folder or on the fridge. Go with them to the pharmacy and ask the pharmacist to explain the changes. Use the “Ask Me 3” questions: What is this for? How do I take it? Why does it matter? Don’t assume they understand-ask them to repeat it back in their own words.
If you’re taking multiple medications, confusion with generics is one of the most preventable risks. The system isn’t perfect-but you don’t have to accept it. Ask questions. Use tools. Speak up. Your health depends on it.
Logan Romine
November 21, 2025 AT 20:03So let me get this straight - we’re spending billions on meds, but the pills look like they were designed by a toddler with a crayon? 🤦♂️
Generics are chemically identical, sure… but if my heart pill turns from white oval to pink round and I don’t know if it’s still my medicine or some Russian knockoff… I’m gonna panic. No amount of ‘health literacy’ fixes bad design. The system is literally gambling with lives. #PillConfusionIsACrime
Chris Vere
November 23, 2025 AT 18:09The issue described is indeed profound and reflects a systemic failure in communication rather than individual deficiency. Health literacy is not merely a personal attribute but a shared responsibility between institutions and citizens. When the appearance of essential medication varies unpredictably without clear guidance, it is unreasonable to expect patients to navigate such ambiguity. Standardization, even in color and shape, would significantly reduce anxiety and error. This is not radical - it is rational.
Mark Kahn
November 24, 2025 AT 21:55Love this post. Seriously. I work with seniors and this is SO real.
One lady thought her blood pressure med changed because it went from blue to green - she stopped taking it for a week and ended up in the hospital. We made her a little card with pics of each version and now she’s fine.
Simple fixes work. Talk to your pharmacist. Keep a list. Use Medisafe. You got this 💪
Swati Jain
November 26, 2025 AT 19:32Let’s be real - this isn’t about literacy, it’s about corporate negligence masked as ‘trademark law.’ The FDA lets pharma companies design pills like cereal boxes - colorful, confusing, and intentionally inconsistent to maximize profit margins. Meanwhile, grandma’s on 12 meds and can’t tell which is which. The ‘Ask Me 3’ program? Cute. But if your system doesn’t standardize pill appearance, you’re just putting a Band-Aid on a hemorrhage. And don’t get me started on the $4.7M ‘improvement’ budget - that’s less than what Big Pharma spends on lobbying in a single afternoon. 🤡
Julia Strothers
November 26, 2025 AT 23:37THIS IS A GLOBALIST SCHEME. Why do you think the pills change? It’s not about trademarks - it’s about tracking you. The CDC, WHO, and Big Pharma are all in bed together. They want you confused so you’ll take MORE pills. They want you scared so you’ll use the Medisafe app - which is probably a spy tool. Look at Australia’s color code - why are they so far ahead? Because they’re NOT part of the globalist agenda. They’re not letting the UN dictate what color your diabetes pill should be. This is control. And you’re letting them win.
Erika Sta. Maria
November 28, 2025 AT 12:39Wait wait wait - you say generics are the same? But I read on a forum that the inactive ingredients can cause different side effects like anxiety or bloating? And what about bioequivalence? Like… 80-125% range? That’s not the same. That’s a range. So technically they’re not identical. Also, why do you assume everyone has a smartphone? My aunt uses a flip phone. And the ‘brown bag’ thing? That’s just more work for nurses who are already overworked. And why are we trusting the FDA? They approved opioids. They approved blood thinners that killed people. You think they care about your pink pill? 🤡
Nikhil Purohit
November 29, 2025 AT 02:54Man I’ve seen this happen with my dad. He’d just stare at the pill like it was a riddle. Then one day I took him to the pharmacy and the pharmacist showed him the bottle label and said ‘same medicine, different maker’ - and he just nodded like it made sense. No app needed. Just someone taking 30 seconds to explain it. Maybe the real solution isn’t color-coding or apps… it’s just better human interaction. Pharmacies should be trained to do this as standard. Not optional. Not ‘extra.’ Just… normal.
David vaughan
December 1, 2025 AT 02:14I’ve been taking metformin for 8 years. The shape changes every 6 months. The color? Always different. I’ve kept a notebook. I write down the shape, the imprint, the color, the pharmacy. I scan it. I cross-reference. I’ve saved 17 different versions. I’ve called my doctor 5 times. I’ve cried once. I’m not paranoid. I’m prepared. And I’m not alone. We need a national database. Not an app. A database. With photos. With barcodes. With manufacturer history. And it needs to be public. Free. Accessible. I’ve started one on Google Sheets. If you want to contribute… I’ll share it. Please. Don’t let this keep happening.