Hashimoto's thyroiditis is the most common cause of hypothyroidism in places where people get enough iodine in their diet. It happens when your immune system mistakenly attacks your thyroid gland - the small butterfly-shaped organ at the base of your neck that controls your metabolism. Over time, this attack damages the gland, reducing its ability to make thyroid hormones. The result? Fatigue, weight gain, cold intolerance, brain fog, and a host of other symptoms that can make daily life feel like a slow grind.
What makes Hashimoto’s tricky isn’t just the symptoms - it’s the way treatment and monitoring work. Unlike other health issues where you feel better right after taking medicine, Hashimoto’s requires patience, precision, and regular blood tests. The key? TSH - thyroid-stimulating hormone. It’s not just a number on a lab report. It’s the most reliable guide to whether your treatment is working.
How Hashimoto’s Turns Into Hypothyroidism
Hashimoto’s doesn’t start with full-blown hypothyroidism. It begins quietly. Your immune system starts producing antibodies - mainly thyroid peroxidase antibodies (TPOAb) - that target enzymes in your thyroid. At first, your thyroid compensates. You might feel fine. Or you might have mild symptoms like occasional tiredness or dry skin. But over months or years, the damage adds up. The gland gets scarred. It can’t keep up. Eventually, hormone levels drop. That’s when TSH rises.
TSH is made by your pituitary gland. When your thyroid isn’t producing enough hormone, the pituitary says, “Hey, we need more!” and pumps out more TSH to push the thyroid into action. So a high TSH is the body’s alarm bell. In fact, according to the American Thyroid Association, TSH is the most reliable marker for diagnosing and managing primary hypothyroidism - and Hashimoto’s is the #1 cause of that.
Diagnosis usually starts with a TSH test. If it’s above 4.5 mIU/L, doctors check free T4 and TPOAb. If T4 is low and TPOAb is high, it’s Hashimoto’s. You don’t need to test T3. You don’t need to repeat antibody tests every few months. Antibodies don’t tell you if your dose is right. They just confirm the autoimmune cause. Once diagnosed, the focus shifts entirely to TSH.
Why TSH Is the Only Number That Matters
Many patients expect their doctor to check free T4 or T3 regularly. But for most people with Hashimoto’s, that’s unnecessary. The Cleveland Clinic, the American Association of Clinical Endocrinologists, and the American Academy of Family Physicians all agree: if you have primary hypothyroidism and no pituitary problems, TSH alone is enough to guide treatment.
Why? Because TSH is incredibly sensitive. It reacts to tiny changes in thyroid hormone levels. Even a small drop in T4 causes TSH to climb. That means it catches under-treatment before symptoms get bad. And when you take too much levothyroxine, TSH drops below normal - often before you feel jittery or have heart palpitations.
There’s a myth that “normal” TSH means 0.4 to 4.0 for everyone. But that’s not true. The normal range is broad. For someone in their 30s, the average TSH is around 1.2. For someone over 65, a TSH of 5.0 might be fine. The goal isn’t to hit the middle of the range. It’s to find the level where you feel your best - while staying safely within guidelines.
Studies show that people with certain gene variations (like the DIO2 polymorphism) do better with a TSH target in the lower half of normal - between 0.4 and 2.0 mIU/L. That’s why some doctors aim for 1.0 to 2.5, especially if you still feel tired or depressed despite being “in range.” Your body’s ideal TSH might be different from your neighbor’s.
Levothyroxine: The Standard Treatment
Levothyroxine (LT4) is the only treatment recommended by major medical groups. It’s a synthetic version of T4, the hormone your thyroid normally makes. Your body converts it to T3, the active form. You don’t need T3 supplements. Most people do fine on LT4 alone.
Dosing starts at about 1.4 to 1.8 mcg per kilogram of body weight. For a 70kg adult, that’s roughly 100 mcg/day. But many doctors start lower - especially in older adults or people with heart conditions. A common starting dose is 25 to 50 mcg. Then you wait.
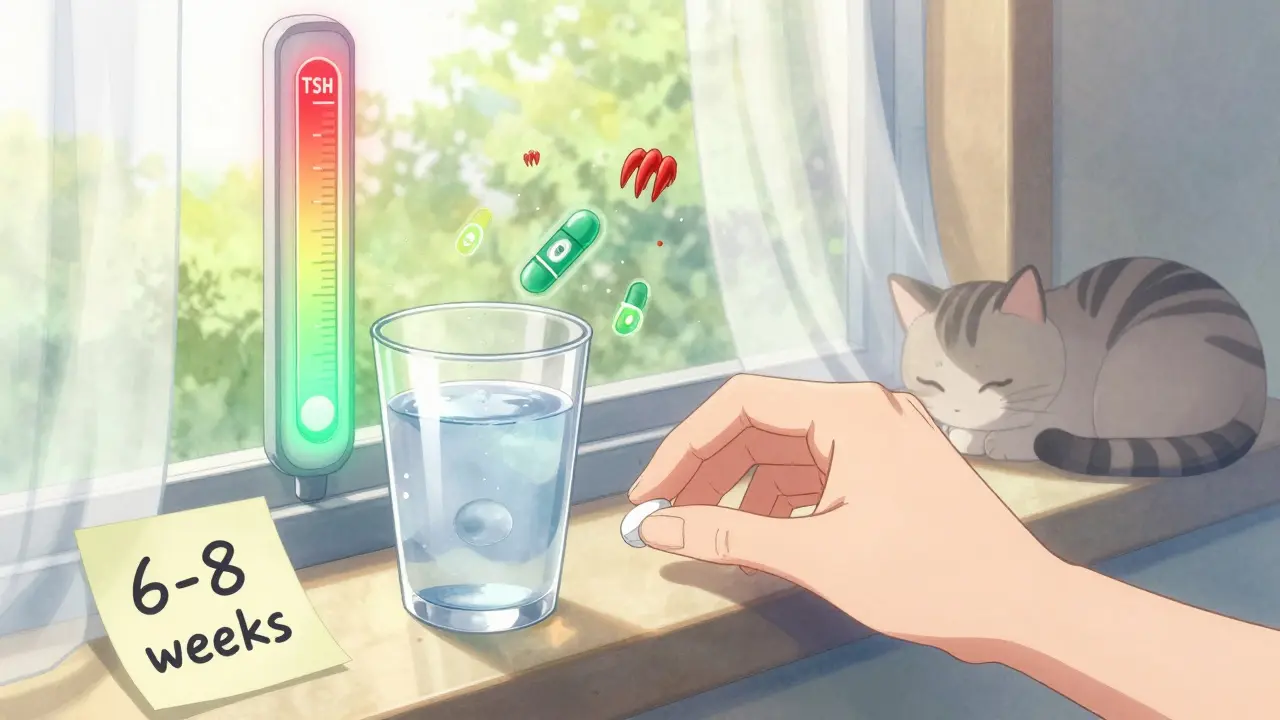
That’s the hard part. You can’t adjust your dose after a week. Levothyroxine has a long half-life. It takes 4 to 6 weeks for your body to fully absorb the change. Another 2 to 4 weeks for your pituitary to respond. So your TSH won’t stabilize until about 6 to 8 weeks after a dose change. That’s why every guideline - from Mayo Clinic to AAFP - says: test at 6 to 8 weeks after starting or changing your dose.
Most people need 2 to 3 dose adjustments before they hit the sweet spot. Some need more. Don’t get discouraged. It’s not you. It’s biology.
When to Test and How Often
Here’s the standard timeline:
- Test TSH 6 to 8 weeks after starting levothyroxine.
- Test again 6 to 8 weeks after any dose change.
- Once your TSH is stable for 6 months, switch to annual testing.
Some clinics test every 4 weeks early on. That’s not wrong, but it’s not more accurate. Testing too soon just gives you confusing numbers. Your TSH won’t have settled yet. You’ll end up adjusting too early - and chasing a moving target.
There are exceptions. If you’re pregnant, you need testing every 4 weeks until week 20. Pregnancy changes how your body handles thyroid hormone. Even if you were stable before, your dose will likely need to increase by 25% to 50%. If you’re planning pregnancy, get your TSH under 2.5 before conceiving - higher levels increase risks of miscarriage and preterm birth.
Other triggers for more frequent testing:
- Starting or stopping iron, calcium, or proton pump inhibitors (like omeprazole)
- Significant weight gain or loss (more than 10% of body weight)
- Switching levothyroxine brands (even generics can vary slightly)
- Starting or stopping estrogen-containing birth control or hormone therapy
These all affect how your body absorbs or uses levothyroxine. Your TSH will drift. Don’t wait for your annual checkup.
What Symptoms Tell You (And What They Don’t)
Feeling tired? Weight gain? Dry skin? Those are classic signs of under-treatment - high TSH. But they’re also common in stress, sleep deprivation, or menopause. Don’t assume your symptoms mean your dose is wrong.
On the flip side: anxiety, heart racing, trouble sleeping? That’s often a sign of too much hormone - low TSH. But again, these can be caused by caffeine, anxiety, or other conditions.
That’s why symptoms alone aren’t enough. They’re clues - not proof. Your doctor should listen to how you feel. But the dose should be adjusted based on TSH, not just how you say you feel. Otherwise, you risk overtreating.
Still, if your TSH is in range and you still feel awful? Talk to your doctor. Some patients benefit from a lower TSH target - even if it’s still “normal.” The American Association of Clinical Endocrinologists says it’s okay to aim for 0.4 to 2.5 mIU/L if you have persistent symptoms. Don’t accept feeling bad just because your numbers are “fine.”
What You Shouldn’t Waste Time On
Don’t test your thyroid antibodies repeatedly. Once they’re high, they stay high. They don’t predict disease progression or treatment success. The American Thyroid Association says it clearly: repeating antibody tests isn’t needed.
Don’t chase T3 supplements. Even if you’re still tired, adding T3 (like Cytomel) hasn’t proven better than levothyroxine alone in large studies. The Cochrane Review found no consistent benefit. Stick with LT4 unless you’re in a research trial.
Don’t stress about the brand. Generic levothyroxine is safe and effective. But if you switch brands and your TSH changes, tell your doctor. Some people are sensitive to tiny differences in fillers. Consistency matters.
Don’t take your pill with coffee, calcium, or iron. Wait at least 60 minutes. These block absorption. Take it on an empty stomach, first thing in the morning, with water.
The Future of Monitoring
There’s exciting stuff coming. In 2021, the FDA approved the first home TSH test - ThyroChek. It’s not widely used yet, but it’s a sign of things to come. Imagine checking your TSH every 2 weeks from your kitchen. That could speed up dose adjustments and reduce the frustration of waiting 8 weeks.
Research is also looking at personalized targets based on genetics, age, and even gut health. We’re moving away from one-size-fits-all. Your ideal TSH might be 1.1. Mine might be 2.3. That’s okay.
For now, though, the rules are simple: test TSH at 6 to 8 weeks after any change. Take your pill the same way every day. Don’t skip doses. And if you’re not feeling better - even with a normal TSH - speak up. Your symptoms matter. You deserve to feel well.

Christine Joy Chicano
January 6, 2026 AT 15:24Hashimoto’s is such a sneaky beast. I was diagnosed five years ago and spent the first year convinced my doctor was just dismissing me because I was a ‘young woman with anxiety.’ Turns out my TSH was 8.7. No joke. I cried in the parking lot after getting the results. Now I’m stable at 1.4 on 112 mcg, and I actually sleep through the night. If you’re tired and your TSH is above 4, don’t wait. Push for a test.
steve rumsford
January 8, 2026 AT 10:45so i took my levothyroxine with my morning coffee like always and now my tsh is 6.2 🤦♂️
Adam Gainski
January 9, 2026 AT 11:48Steve, that’s actually super common. Coffee, especially black, can block up to 30% absorption if taken within an hour. I used to do the same thing. Switched to taking mine at bedtime with water-no food, no caffeine, no calcium-and my TSH dropped from 5.8 to 1.9 in 8 weeks. It’s not magic, it’s just biology. Consistency is everything.
Poppy Newman
January 9, 2026 AT 13:24Thank you for this. I’ve been reading everything I can since my diagnosis last month. I was terrified I’d never feel like myself again. Now I feel like I have a roadmap. 💪
Mina Murray
January 9, 2026 AT 16:31They say TSH is the only number that matters. But have you seen the labs from the CDC? They’ve been quietly adjusting the ‘normal’ range since 2010 to make more people ‘normal.’ Why? Because Big Pharma makes billions off levothyroxine. Your TSH might be ‘normal’ but you’re still exhausted because your T3 conversion is broken. Nobody talks about DIO2 polymorphisms because it’s not profitable to treat you with T3. They want you dependent on a pill that doesn’t fix the root cause.
Andrew N
January 10, 2026 AT 23:10That’s a conspiracy theory. TSH is the most sensitive marker we have. Studies show T3 supplementation doesn’t improve outcomes in controlled trials. The Cochrane Review says so. You’re ignoring evidence because you want to believe there’s a secret fix. You’re not special. Your body doesn’t need magic. It needs consistent dosing.
Kyle King
January 12, 2026 AT 17:19So you're saying the FDA approves home TSH tests but we're not supposed to question why they only approved one brand? And why is it still not covered by insurance? This is all a setup. They want you to keep going back to the clinic so they can keep billing. They don't want you to be independent. They want you hooked. You think your doctor cares? They're paid per visit. You're a revenue stream.
Vince Nairn
January 14, 2026 AT 05:19Wow. So we’ve got the conspiracy guy, the evidence guy, and now the guy who thinks the medical system is a pyramid scheme. I just want to take my pill and not feel like a zombie. Can we all just agree that 6-8 weeks is too long to wait for a lab result? Can we get a damn app that reminds us to take our meds and not drink coffee for an hour? That’s the real win.
Jessie Ann Lambrecht
January 15, 2026 AT 04:12To everyone freaking out about T3 or conspiracy theories: your symptoms matter. If your TSH is ‘in range’ and you’re still exhausted, depressed, or foggy - tell your doctor. Push for a target of 0.5–2.0. It’s not radical. It’s evidence-based. The AACE says so. You’re not being difficult. You’re being your own advocate. And that’s brave. Don’t let anyone make you feel silly for wanting to feel human again.
Kamlesh Chauhan
January 16, 2026 AT 16:32my tsh was 12 and my doctor said im fine because im not obese and i dont have hair loss yet i cried for 3 days straight and now i take my meds in the shower because i forget and i still feel like death and my cat judges me
Ayodeji Williams
January 18, 2026 AT 13:16bro why are you all so serious? just take your pill and vibe. if you feel bad maybe you need more sun or less stress or a new girlfriend. thyroid is just a vibe check. also i switched to kelp supplements and now i glow
Elen Pihlap
January 18, 2026 AT 17:28i’ve been on levothyroxine for 12 years and i still feel like a ghost. everyone says ‘just take your pill’ but no one says ‘what if your body just doesn’t want to work anymore?’ i’m tired of being told i’m not trying hard enough. i’m just tired.