When you pick up a prescription, you might see two versions of the same medicine: one with a familiar brand name, and another with a plain chemical name. If you’ve ever wondered whether the cheaper one works just as well, the answer is yes - generic drugs are not second-rate. They’re the exact same medicine, made to the same strict standards, but without the marketing costs that drive up brand-name prices.
What Exactly Is a Generic Drug?
A generic drug is a copy of a brand-name medication that becomes available after the original patent expires. Patents usually last 20 years, giving the original maker time to recover research costs. Once that window closes, other companies can make the same drug using the same active ingredient. The U.S. Food and Drug Administration (FDA) defines a generic drug as one that is identical or bioequivalent to the brand-name version in dosage, safety, strength, how it’s taken, quality, performance, and intended use. It’s not a copy in the way a knockoff handbag is a copy. It’s not a cheaper version with less punch. It’s the same medicine, made to the same exact rules. The FDA requires that every generic drug deliver the same amount of active ingredient into your bloodstream at the same rate as the brand-name version. This is called bioequivalence - and it’s not a suggestion. It’s a legal requirement.How Are Generic Drugs Approved?
Getting a new drug approved used to mean running full clinical trials - testing on animals, then hundreds or thousands of people. That cost an average of $2.6 billion per drug. Generic manufacturers don’t have to do that. Instead, they use a faster, cheaper path called the Abbreviated New Drug Application (ANDA). Here’s how it works: the company proves two things. First, that their drug has the same active ingredient, strength, dosage form (tablet, capsule, liquid, etc.), and route of administration (oral, injected, etc.) as the original. Second, that it behaves the same way in the body. That second part is tested in small studies with 24 to 36 healthy volunteers. Blood samples are taken over time to measure how much of the drug enters the bloodstream and how fast. The results must fall within 80% to 125% of the brand-name drug’s levels. If it’s outside that range, the FDA rejects it. The FDA inspects every manufacturing facility - whether it’s in the U.S., India, or China - to make sure it follows Current Good Manufacturing Practices (cGMP). These are the same rules applied to brand-name factories. In 2023 alone, the FDA conducted about 3,500 inspections of generic drug plants worldwide. No exceptions.Are Generic Drugs Really the Same?
Yes. But here’s where people get confused: they look different. Generic drugs often have different colors, shapes, or flavors. That’s because trademark laws require them to look different from the brand-name version. The active ingredient? Identical. The way it works in your body? Identical. The inactive ingredients - like fillers, dyes, or preservatives - might be different. But those don’t affect how the medicine works. They’re chosen for stability, cost, or to make the pill easier to swallow. The FDA has reviewed hundreds of studies comparing generics and brand-name drugs. One major review by the Institute of Medicine looked at 38 clinical trials on cardiovascular drugs and found no meaningful difference in effectiveness. The American Medical Association, the American College of Physicians, and the FDA all agree: generics are just as safe and effective. Dr. Janet Woodcock, former head of the FDA’s drug division, put it plainly: “The FDA would not allow generics to be marketed unless they were therapeutically equivalent to the brand.”Why Are Generic Drugs So Much Cheaper?
Because they don’t have to pay for research, marketing, or advertising. The original drug company spent years and billions developing the medicine, running trials, and promoting it. Once the patent expires, other companies can jump in. They don’t need to repeat all that work. They just need to prove they make the same thing. That’s why generics cost 80% to 85% less. In the U.S., generics make up 90% of all prescriptions filled - but only 13% of total drug spending. Over the past decade, they’ve saved the healthcare system more than $2 trillion. When more than five companies start making the same generic, prices can drop even further - sometimes to just 9% of the original brand price. That’s the power of competition.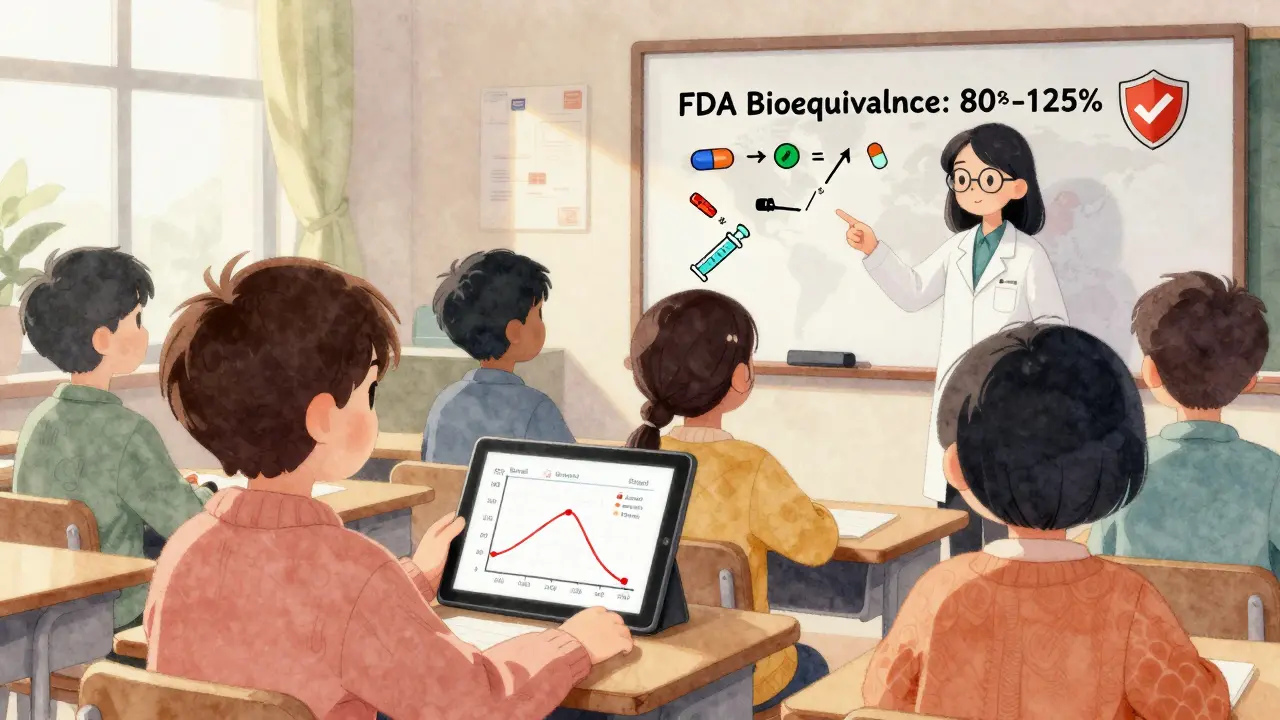
What About Complex Drugs Like Biologics?
Not all drugs are easy to copy. Biologics - drugs made from living cells, like insulin, rheumatoid arthritis treatments, or cancer therapies - are far more complex than pills. You can’t just mix chemicals in a lab and get the same result. For these, the FDA created a separate category called biosimilars. They’re not exact copies. They’re “highly similar” to the original, with no clinically meaningful differences. But because they’re harder to replicate, they don’t save as much. Biosimilars typically cost 20% to 30% less, not 80%. And they’ve been slower to catch on - only about 31% of potential market share had been captured by 2022.Are There Any Risks?
For most people, no. But there’s one group where switching can be trickier: people taking drugs with a narrow therapeutic index. These are medicines where even a small change in blood levels can cause problems. Examples include warfarin (a blood thinner), levothyroxine (for thyroid issues), and some epilepsy drugs. In these cases, doctors may prefer to stick with one version - brand or generic - to avoid any possible fluctuation. But even here, studies show that switching between approved generics and brand-name versions doesn’t lead to worse outcomes for most patients. The key is communication with your doctor or pharmacist. If you’re concerned, ask if your drug falls into this category.How Do You Know If You’re Getting a Generic?
Your prescription label will list the generic name first - the chemical name, like “metformin” or “amlodipine.” The brand name, like “Glucophage” or “Norvasc,” might be listed too, but it’s usually smaller. Your pharmacist is required to substitute a generic unless your doctor writes “dispense as written” on the prescription. In 49 U.S. states, pharmacists can switch to a generic automatically. If you’re unsure, ask. Pharmacists are trained to explain the difference. They’ll tell you the generic looks different, but works the same. Many even keep side-by-side pictures on hand to show patients.
What’s Next for Generic Drugs?
More than 350 brand-name drugs are set to lose patent protection between 2023 and 2027. That means a wave of new generics will hit the market, potentially saving billions more. But there are challenges. Eighty percent of the active ingredients in generics come from just two countries: India and China. Supply chain issues, like those seen during the pandemic, can lead to shortages. The FDA is working to fix that. New rules under GDUFA III aim to speed up approvals and increase inspections in foreign facilities. The agency is also paying more attention to complex generics - things like inhalers, eye drops, and topical creams - which are harder to copy than pills. Meanwhile, some brand-name companies are launching their own generics - called “authorized generics.” These are made by the original company but sold under a generic label. They’re identical to the brand, but priced lower to compete with other generics.Bottom Line
Generic drugs aren’t a compromise. They’re the smart choice. They save money without sacrificing safety or effectiveness. The science is clear. The regulators are strict. And the evidence shows they work just as well. If your doctor prescribes a brand-name drug, ask: “Is there a generic?” If you’re paying out of pocket, the savings can be hundreds - even thousands - of dollars a year. That’s not just a financial win. It’s a health win.Are generic drugs as effective as brand-name drugs?
Yes. Generic drugs must meet the same FDA standards as brand-name drugs. They contain the same active ingredient, in the same strength and dosage form, and must prove bioequivalence - meaning they deliver the same amount of medicine into your bloodstream at the same rate. Thousands of studies confirm they work just as well.
Why do generic drugs look different?
Trademark laws require generic drugs to look different from brand-name versions - so they can’t be confused with the original. That means different colors, shapes, or sizes. But the active ingredient and how it works in your body are identical. The differences are only in inactive ingredients like dyes or fillers, which don’t affect effectiveness.
Are generic drugs made in the same kind of facilities as brand-name drugs?
Yes. The FDA inspects all drug manufacturing facilities - brand and generic - using the same strict rules called Current Good Manufacturing Practices (cGMP). In 2023, the agency conducted over 3,500 inspections worldwide. A generic drug plant in India or China must meet the same quality standards as one in the U.S.
Can I switch from a brand-name drug to a generic safely?
For most medications, yes. Switching is safe and common. But for drugs with a narrow therapeutic index - like warfarin, levothyroxine, or certain seizure meds - small changes in blood levels can matter. Talk to your doctor before switching. They may recommend sticking with one version to avoid any risk.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to pay for expensive research, clinical trials, or marketing. Once a patent expires, multiple companies can make the drug, driving prices down through competition. The original brand-name drug company spent an average of $2.6 billion to develop the medicine - generics skip those costs.
Do generic drugs have the same side effects as brand-name drugs?
Yes. Since they contain the same active ingredient and work the same way in the body, side effects are identical. Any differences in side effects reported by patients are usually due to variations in inactive ingredients - like fillers or dyes - which rarely cause reactions. If you notice a change after switching, talk to your pharmacist or doctor.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs - pills you swallow. Biosimilars are copies of biologics - complex drugs made from living cells, like insulin or cancer treatments. Because biologics are so complex, biosimilars can’t be exact copies. They’re “highly similar” and must show no meaningful difference in safety or effectiveness, but they’re not identical. That’s why they cost less, but not as much as traditional generics.
How do I know if my prescription is a generic?
Check the label. The generic name - the chemical name like “metoprolol” or “fluoxetine” - will be listed first. The brand name, like “Lopressor” or “Prozac,” may appear below it in smaller text. Your pharmacist can also tell you. In most states, they’re allowed to substitute a generic unless your doctor says “dispense as written.”

Amber Lane
January 20, 2026 AT 03:06My grandma switched to generics for her blood pressure med and saved $400 a year. She didn’t notice any difference - just cheaper pills that did the same job.
Ben McKibbin
January 21, 2026 AT 10:57Let’s be real - the pharmaceutical industry’s whole business model is built on exploiting patent cliffs. Brand-name drugs are a luxury tax disguised as innovation. Generics aren’t ‘just as good’ - they’re the *only* version that should ever be prescribed unless there’s a proven, documented clinical exception. The fact that we still pay premium prices for branded versions in 2024 is a moral failure.
The FDA doesn’t just ‘approve’ generics - they enforce bioequivalence with surgical precision. If your doctor says ‘stick with the brand,’ ask them if they’re getting kickbacks. Spoiler: they’re not. They’re just lazy or misinformed.
And yes, the color change freaks people out. But that’s trademark law, not science. You wouldn’t refuse a different brand of aspirin because it’s blue instead of white. Why treat heart meds like sacred artifacts?
The real scandal? Authorized generics. Big pharma making their own generics to corner the market and pretend they’re ‘competing.’ It’s corporate theater. The patient wins either way - but the system is rigged to make us feel guilty for saving money.
Stephen Rock
January 23, 2026 AT 02:52so like… generics are just as good but look different and sometimes make me feel weird but its fine
also why do they always taste like cardboard
also my cousin took a generic and cried for 3 hours
idk man
shubham rathee
January 24, 2026 AT 12:28you know what they dont tell you right the FDA only inspects 1 in 10 plants in india and china and most of the active ingredients are made in facilities with no running water
and the bioequivalence studies are done on 24 college kids who get paid in free pizza
and the 80-125% range is basically saying your drug could be half as strong or 25% stronger and still pass
they call it science but its just corporate propaganda
and dont get me started on the chinese labs that got caught dumping chemicals into rivers and still got approved
Philip Williams
January 25, 2026 AT 01:43It's worth noting that the FDA’s bioequivalence standards are among the most rigorous in the world - far exceeding those of many other regulatory bodies. The 80–125% confidence interval isn’t arbitrary; it’s statistically validated across thousands of trials. What’s more, the agency requires that generics demonstrate not just average equivalence, but also consistent performance across individual patients - meaning variability must be tightly controlled.
Additionally, the fact that over 90% of prescriptions in the U.S. are filled with generics, while accounting for only 13% of total spending, underscores their critical role in sustaining healthcare accessibility. Without them, millions would be forced to choose between medication and basic necessities.
It’s also important to distinguish between generic small-molecule drugs and biosimilars. The former are chemically identical; the latter are complex biological products with inherent variability. Conflating the two misrepresents the science and undermines public trust.
Finally, the notion that ‘different-looking pills = different effects’ is a psychological bias, not a pharmacological reality. The inert ingredients - colorants, binders, coatings - are chosen for manufacturability and stability, not efficacy. If you experience a change in side effects after switching, it’s more likely due to placebo effect or unrelated factors.
The bottom line: generics are not a compromise. They are the standard of care - and the most equitable solution in modern medicine.
Andrew Rinaldi
January 25, 2026 AT 18:04I’ve been on the same generic thyroid med for 8 years. My doctor switched me from brand to generic when I was uninsured. I’ve had zero issues. No weight changes, no fatigue spikes, no weird side effects. My labs are rock steady.
I think the fear around generics comes from how little most people know about how drugs are made. We’re taught to trust big names - Nike, Apple, Pfizer. But medicine doesn’t work like sneakers. The chemistry doesn’t care who printed the label.
It’s kind of beautiful, really. Someone in a factory in Hyderabad makes a pill that’s chemically identical to the one made in New Jersey. And it works the same. No marketing, no branding, just science.
Maybe the real question isn’t ‘are generics safe?’ but ‘why do we still let companies charge $500 for a drug that costs $2 to make?’
Kevin Narvaes
January 27, 2026 AT 03:59bro i took a generic version of my anxiety med and i swear i felt like i was melting into the couch for 3 days
then i switched back to the brand and boom instant clarity
theyre not the same trust me
also the generic looked like a gummy bear
Ashok Sakra
January 28, 2026 AT 01:55you think generics are safe? in india they make them in basements with dirty water
my uncle took one and his skin turned green
they are poisoning us
why dont you take the brand name and stop being cheap