Every year, thousands of patients in the U.S. are forced to wait for life-saving medications - not because they can’t afford them, but because there simply aren’t enough pills, injections, or IV bags to go around. Generic drug shortages aren’t rare glitches. They’re systemic failures that hit hospitals, pharmacies, and homes with quiet, dangerous frequency.
Why Generic Drugs Are the Most Vulnerable
Generic drugs make up 90% of all prescriptions filled in the U.S. But they’re also behind nearly 70% of all drug shortages. Why? It comes down to money. These drugs cost pennies. A vial of generic vancomycin might sell for $1.50. The manufacturer barely breaks even after production, shipping, and regulatory compliance. That’s a far cry from brand-name drugs, which can earn 30-40% profit margins. Generic makers operate on 5-10% margins - sometimes less.When profit is this thin, companies don’t invest in extra capacity. They don’t build backup lines. They don’t stockpile raw materials. One broken machine. One FDA inspection failure. One supplier in China halting exports - and the entire supply vanishes.
Over 70% of generic drugs have only one or two manufacturers approved by the FDA. That’s not competition. That’s a single point of failure. If one plant shuts down - whether because of quality issues, natural disaster, or financial loss - there’s no one else to step in. And because these drugs are cheap, no one wants to risk money entering the market.
Where the Supply Chain Breaks Down
Most people think of drugs as being made in the U.S. But over 80% of the active ingredients in generic medicines come from factories in China and India. The rest of the production - mixing, filling, sterilizing - often happens in a handful of specialized plants scattered across the globe.Sterile injectables - like antibiotics, chemotherapy drugs, and IV fluids - are the worst hit. Why? They require clean rooms, complex equipment, and exacting standards. A single speck of dust can ruin a batch. These facilities are expensive to build and maintain. Only a few companies have them. And when one fails - like the 2023 shutdown of a major sterile injectable plant in Puerto Rico - the ripple effect hits every hospital in the country.
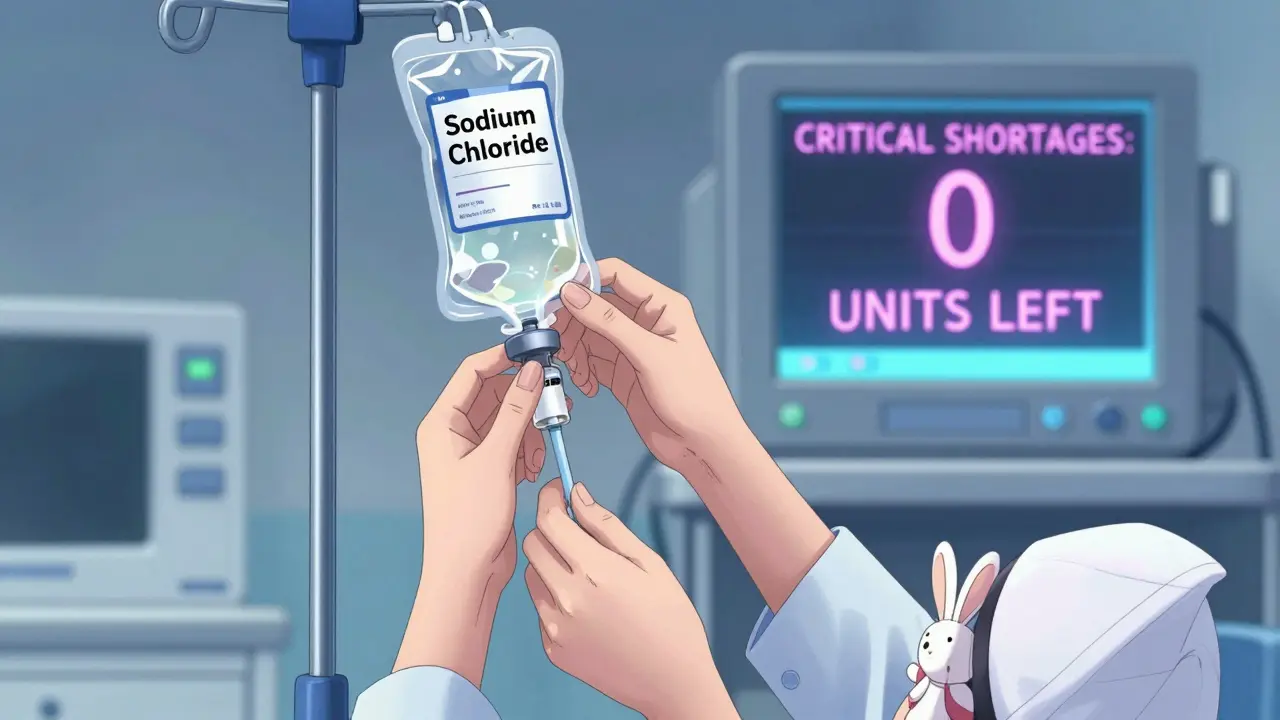
Even the raw materials aren’t safe. In 2024, a shortage of sodium chloride (saline) spiked after a supplier in India faced quality issues. Within weeks, hospitals were rationing IV fluids. Patients with dehydration, kidney failure, or cancer were delayed or switched to riskier alternatives.
The Human Cost of Empty Shelves
It’s easy to talk about numbers - 270 active shortages as of April 2025, 24-month median duration - but behind each number is a patient.Hospitals report that 89% have had to delay treatments because of shortages. Cancer centers say 67% have changed chemotherapy regimens because cisplatin or doxorubicin wasn’t available. Pharmacists spend 15-20 hours a week just tracking down substitutes. That’s time not spent counseling patients, checking for interactions, or catching errors.
On Reddit, a pharmacist wrote: “We’ve been out of vancomycin powder for eight months. We’re using alternatives that are less effective, more toxic, and 10 times more expensive. Patients are getting sicker because we can’t give them the right drug.”
Patients with chronic pain are being denied refills because opioids like morphine are in short supply. Diabetics are switching from insulin analogs to older, less predictable forms. Newborns in NICUs are getting diluted or delayed antibiotics because sterile injectables are gone.
And it’s not just about availability. When a drug is scarce, prices spike. A generic drug that cost $20 a month might jump to $80 - not because the cost of production changed, but because demand outstrips supply. Patients abandon prescriptions. They skip doses. They go to emergency rooms because they can’t manage their condition at home.
Why Brand Drugs Don’t Face the Same Crisis
You might think brand-name drugs are just as bad. They’re not. Between 2018 and 2023, there were 1,391 generic drug shortages - but only 600 for brand-name drugs. Why the difference?Brand drugs have pricing power. Companies can raise prices to cover costs, invest in backup production, or pay more for reliable suppliers. They also have more therapeutic alternatives. If one brand of blood pressure pill is out, a doctor can switch to another brand - same active ingredient, different name.
For generics, that’s not an option. If you’re out of metformin 500mg, you can’t just swap in another generic. They’re not interchangeable in the eyes of insurance or pharmacy systems. And often, there’s no brand alternative at all. The drug is too old. Too cheap. No company makes a branded version.
Even when alternatives exist, they’re often worse. A 2024 HHS report found that patients on substituted generic drugs had a 37.6% drop in medication fills - compared to 30.4% for brand-name drugs. That means more people stop taking their meds entirely.
Manufacturing Is Disappearing
The U.S. used to have over 1,800 facilities making generic drugs. By 2024, that number dropped to 1,437 - a 22% decline in just nine years. Why? Because it’s not profitable anymore.Generic drug margins have fallen from 35% in 2010 to 18% in 2024. Companies are closing plants, consolidating operations, and moving production overseas - even though that makes the supply chain more fragile. The top 10 manufacturers now control 60% of the market. That’s not competition. It’s a monopoly of scarcity.
Meanwhile, FDA inspections are finding more quality issues. Citations for manufacturing violations rose 35% from 2020 to 2024. Plants are being shut down for poor sanitation, inaccurate labeling, or failing to meet sterility standards. But when a plant closes, no one replaces it. The system doesn’t reward rebuilding.

What’s Being Done - And Why It’s Not Enough
The FDA launched a Drug Shortage Task Force in 2024 with four goals: diversify manufacturing, create financial incentives, use advanced tech, and improve early warnings. Some progress has been made. After President Biden signed Executive Order 14050 in 2020, shortages of essential medicines dropped 32% - until 2023, when they started climbing again.But the core problem remains: the market rewards the lowest price, not the most reliable supply. As Dr. Valerie Malta from the University of Utah says, “Low-priced drugs are more vulnerable because they don’t generate enough revenue to invest in quality or redundancy.”
Proposed tariffs on drug imports from China and India could make things worse. SVB Securities warned in early 2025 that tariffs of 50-200% could disrupt the supply of chemotherapy drugs, saline, and antibiotics - exactly the ones already in short supply.
The Congressional Budget Office predicts shortages will hit 350 by the end of 2026. Two-thirds of those will be sterile injectables - the kind you get in a hospital, not at a pharmacy counter.
What This Means for You
If you take a generic drug - and most people do - you’re at risk. Not because you’re doing something wrong. But because the system is broken.Here’s what you can do:
- Ask your pharmacist if your medication is in short supply. They track this daily.
- If your drug is unavailable, ask if there’s a therapeutically equivalent brand - even if it costs more. Some insurers will cover it if there’s no alternative.
- Don’t skip doses. If you’re out, call your doctor. There’s often a plan.
- Keep a list of your medications, including generic names and dosages. This helps your provider find alternatives faster.
This isn’t about blaming patients. It’s about recognizing a broken system. The same drugs that save lives are being lost because no one is paid to make them reliably. Until that changes, shortages won’t disappear. They’ll just get worse.
Healthcare isn’t just about doctors and hospitals. It’s about factories, supply chains, and pricing rules that no one talks about. And right now, those rules are putting lives at risk.

Patty Walters
January 10, 2026 AT 12:32I work ER triage and we’ve been out of generic morphine for 5 months. Patients with broken ribs? We give them acetaminophen and hope. It’s not okay. I don’t care what the CFO says about margins - people are suffering because we can’t afford to make the cheapest drugs.
And don’t get me started on saline. My kid had a UTI last winter and we waited 3 hours because the hospital was rationing IV bags. Just… wow.
Jenci Spradlin
January 12, 2026 AT 04:06generic vancomycin out since last fall. we’re using teicoplanin now - 10x the cost, and half the docs know how to dose it. pharmacists are basically playing guess-the-dose every shift. nobody’s getting paid enough to deal with this mess.
also, the FDA keeps shutting down plants for ‘microbial contamination’ but never asks why the same plants keep failing. it’s like blaming a broken faucet when the whole plumbing system’s rusted.
Elisha Muwanga
January 14, 2026 AT 02:31This is what happens when you outsource everything to communist countries. China doesn’t care if your grandma dies because her antibiotics are late. They care about profit. We used to make drugs here. Now we’re begging for vials like we’re in a third-world country. Shameful.
Build plants in America. Tariff everything from India and China. End of story.
Maggie Noe
January 15, 2026 AT 04:33it’s not just about money. it’s about how we value life. we’ll pay $10k for a cancer drug with a 3% survival bump, but won’t pay $0.50 for a lifesaving antibiotic?
we’ve turned healthcare into a spreadsheet. 🤕
and now we’re surprised when the numbers start bleeding?
we need to ask ourselves: what kind of society lets a child go without antibiotics because the factory in Gujarat had a power outage?
we’re not just failing systems. we’re failing each other.
Catherine Scutt
January 15, 2026 AT 11:14so let me get this straight - we let a handful of companies control 60% of the generic market, then act shocked when they collapse under pressure? 🤦♀️
you think this is new? this has been brewing since 2012. everyone knew. nobody did anything. now you’re mad? grow up.
Darren McGuff
January 16, 2026 AT 00:49I’ve seen this in the UK too - but worse. Our NHS got hit with vancomycin shortages last year and had to import from Brazil because India’s quality control was a joke. We’re all connected now. A plant in Chennai shuts down, and a kid in Manchester gets delayed chemo.
It’s not an American problem. It’s a global failure of accountability. We treat medicine like toilet paper - cheap, disposable, replaceable. Until it’s not.
Alicia Hasö
January 16, 2026 AT 08:29To every person reading this: if you’re on a generic medication, please, write to your representative. Call your senator. Don’t wait until your insulin is gone or your blood pressure meds vanish.
This isn’t politics. It’s survival. And we are the ones who hold the power - not the CEOs, not the FDA, not the Chinese factories.
Our voices matter. Use them.
💙
Drew Pearlman
January 17, 2026 AT 16:14you know what’s wild? we’ve got robots that can land on Mars, but we can’t reliably make a sterile saline bag. think about that.
we’ve got AI that writes poetry, but we can’t predict when a batch of antibiotics will fail because a worker in Hyderabad missed a cleaning protocol.
we’ve got the tech. we’ve got the knowledge. we’ve got the money.
what we don’t have is the will.
and that’s the real tragedy.
we could fix this tomorrow if we chose to. but we keep choosing the lowest bid. again. and again. and again.
it’s not a supply chain issue.
it’s a soul issue.
Chris Kauwe
January 18, 2026 AT 18:04the structural inefficiencies inherent in the generic pharmaceutical value chain are exacerbated by neoliberal market logic - wherein price elasticity is prioritized over systemic resilience, creating a classic tragedy of the commons scenario.
the absence of economies of scale in redundant manufacturing infrastructure, coupled with regulatory capture by oligopolistic actors, has engendered a brittle, monolithic supply architecture - vulnerable to exogenous shocks.
what’s needed is a public-private consortium modeled after the Defense Production Act, with tiered reimbursement incentives tied to inventory buffer thresholds and GMP compliance audits.
otherwise, we’re just rearranging deck chairs on the Titanic.
RAJAT KD
January 20, 2026 AT 17:09India makes 80% of the world’s generics. Shutting us down won’t fix anything - it’ll just make you pay more and wait longer. We’re not the problem. The system is.
Fix the pricing. Fix the incentives. Don’t blame the makers.