Drospirenone is a synthetic progestin used in many combined oral contraceptives (COCs). It mimics natural progesterone, blocks mineralocorticoid receptors, and has anti‑androgenic properties, which makes it popular for acne‑prone and fluid‑retention‑sensitive women. While praised for its skin‑friendly profile, concerns linger about its link to ovarian cysts fluid‑filled sacs that develop on or inside the ovaries. This article untangles the science, weighs the risks, and offers practical steps for anyone taking a drospirenone‑containing pill.
Key Takeaways
- Drospirenone’s anti‑androgenic and aldosterone‑blocking actions can influence cyst formation, but the overall risk is modest.
- Most cysts linked to drospirenone are functional (follicular or luteal) and resolve without treatment.
- Regular ultrasound monitoring is advised only for women with prior cyst history or unexplained pelvic pain.
- Switching to a lower‑risk progestin, such as levonorgestrel, may be considered if cysts become recurrent.
- Lifestyle factors-weight, smoking, and stress-play a bigger role in cyst development than the choice of progestin alone.
How Drospirenone Works Inside the Body
Drospirenone binds to progesterone receptors to suppress ovulation. At the same time, it blocks mineralocorticoid receptors, reducing water retention, and antagonises androgen receptors, lowering acne. The typical combined oral contraceptive contains drospirenone 3mg plus ethinyl estradiol 20µg follows a 21‑day active phase and 7‑day placebo break.
Because ovulation is inhibited, the normal surge of luteinising hormone (LH) that triggers follicle rupture is blunted. In theory, this should decrease the formation of functional cysts that arise from incomplete follicular release. However, the hormonal milieu created by drospirenone can sometimes lead to atypical cyst growth, especially in women with underlying ovarian conditions.
Understanding Ovarian Cysts: Types and Causes
Ovarian cysts fall into two broad categories:
- Functional cysts - develop as part of the menstrual cycle. Follicular cysts form when a follicle fails to rupture; luteal cysts arise after ovulation if the corpus luteum seals off fluid.
- Pathological cysts - include dermoid cysts, endometriomas, and cystadenomas, which are unrelated to hormonal contraception.
Functional cysts are the most common, affecting up to 25% of women of reproductive age at some point. They are usually asymptomatic and resolve within a few weeks. The key symptom that prompts medical attention is persistent pelvic pain or a sudden increase in abdominal girth.
Drospirenone and Cyst Risk: What the Data Say
Several large‑scale studies have examined cyst incidence among drospirenone users:
- A 2022 prospective cohort of 5,800 women found a 3.2% rate of ultrasound‑detected cysts larger than 3cm in drospirenone users, versus 2.1% in levonorgestrel users.
- A meta‑analysis of 12 randomized trials (n≈9,400) reported a relative risk of 1.15 (95% CI 0.98-1.34) for cyst formation with drospirenone‑containing COCs, which is not statistically significant.
- Women with polycystic ovary syndrome (PCOS) or a prior cyst history showed a slightly higher incremental risk (≈5% absolute increase).
In plain language: drospirenone may raise the odds of developing a cyst by a small margin, but most of those cysts are benign and disappear on their own.
Comparing Progestins: Drospirenone vs. Levonorgestrel vs. Desogestrel
| Progestin | Androgenic Activity | Mineralocorticoid Antagonism | Typical Estrogen Dose (µg EE) | Reported Cyst Risk |
|---|---|---|---|---|
| Drospirenone | Low (anti‑androgenic) | Strong | 20‑30 | 3‑4% (functional cysts) |
| Levonorgestrel | Moderate (androgenic) | None | 30‑35 | 2‑3% (functional cysts) |
| Desogestrel | Low | None | 20‑30 | 2‑3% (functional cysts) |
The table shows that drospirenone’s unique mineralocorticoid blocking does not dramatically alter cyst risk compared with other low‑androgenic progestins. Choice should therefore hinge on other factors-acne, mood, blood pressure, and personal preference.
Clinical Guidance: Detecting and Managing Cysts While on Drospirenone
For most women, routine pelvic ultrasounds are unnecessary. Follow these steps if you suspect a cyst:
- Assess symptoms. Sudden, sharp pelvic pain, bloating, or a feeling of heaviness warrants evaluation.
- Schedule an ultrasound. A transvaginal scan can differentiate a simple functional cyst from a complex mass.
- Interpret size. Cysts < 5cm usually resolve within 2‑3months. Larger cysts may need closer follow‑up.
- Decide on continuation. If the cyst is uncomplicated, most clinicians recommend continuing the current COC and re‑scanning in 6‑8weeks.
- Consider switching. Recurrent cysts (>2times/year) or cysts persisting beyond 3months may prompt a switch to a progestin with lower reported cyst association, such as levonorgestrel.
- Address underlying conditions. PCOS, endometriosis, or hypothyroidism can amplify cyst formation; treat these accordingly.
Never ignore severe, sudden pain-it could signal ovarian torsion, a surgical emergency.
Impact on Fertility and Future Pregnancy
Drospirenone does not impair long‑term fertility. Ovulation typically resumes within 4‑6weeks after stopping the pill. For women planning conception, a pre‑conception ultrasound can confirm that any residual cyst has resolved, ensuring a smoother start to pregnancy.
Related Topics and Next Steps in Your Hormonal Health Journey
Understanding drospirenone and cysts opens doors to broader discussions:
- PCOS a hormonal disorder that often presents with multiple ovarian cysts - lifestyle, metformin, and specific COCs can improve symptoms.
- Endometriosis tissue similar to uterine lining grows outside the uterus, sometimes forming chocolate cysts - hormonal suppression may relieve pain.
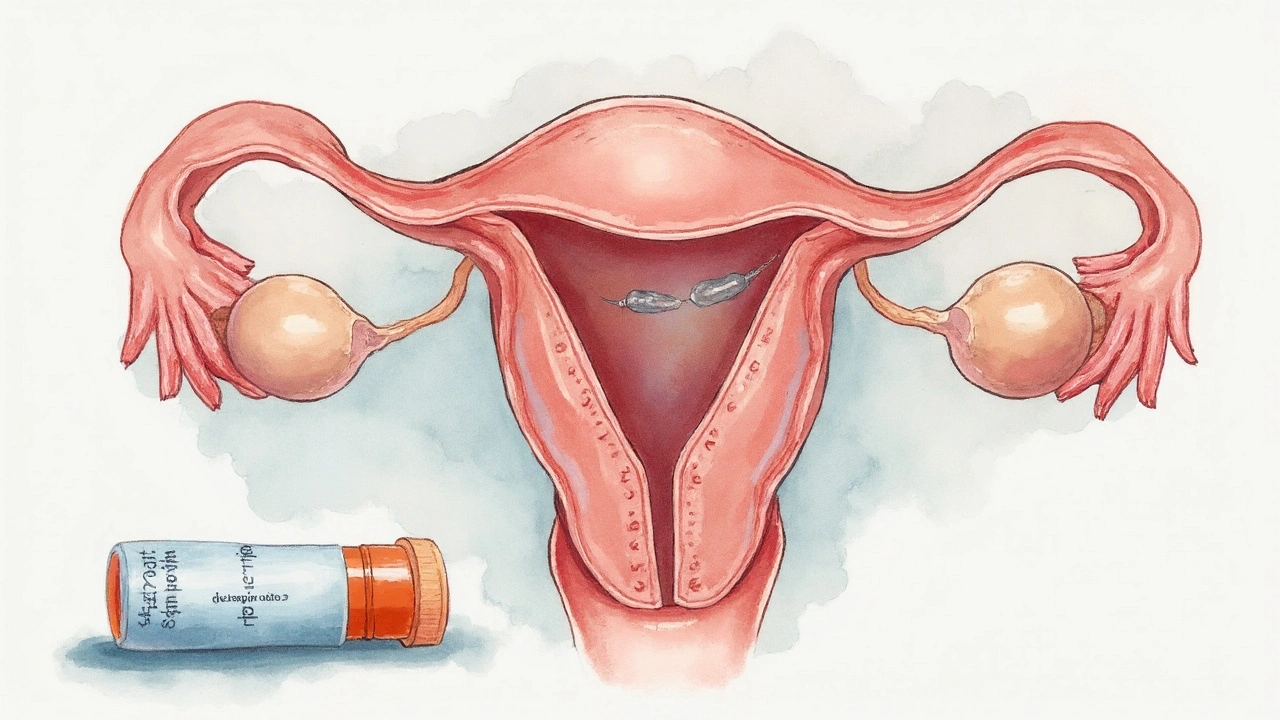
- Non‑oral routes (patch, ring, IUD) that use different progestins and may carry distinct cyst risk profiles.
- Natural family planning and fertility‑awareness methods for those who prefer hormone‑free options.
Each of these areas deserves its own deep dive. If you’ve read this far, consider exploring a follow‑up article on "Managing PCOS with Hormonal Contraceptives" or "Choosing the Right Non‑Oral Birth Control for Cyst Concerns".

Frequently Asked Questions
Can drospirenone cause ovarian cysts?
Drospirenone may slightly increase the odds of developing a functional ovarian cyst, but most cysts are benign, small, and resolve without intervention.
How do I know if a cyst is serious?
Warning signs include severe, sudden pelvic pain, fever, or a rapidly enlarging abdomen. An ultrasound can differentiate a simple cyst from a complex or torsed ovary, which requires urgent care.
Should I switch to another birth control if I get a cyst?
If cysts recur despite treatment, a switch to a progestin with a slightly lower cyst association-such as levonorgestrel-can be discussed with your clinician. However, many doctors advise staying on the current pill if the cyst is uncomplicated.
Do lifestyle factors affect cyst formation?
Yes. Obesity, smoking, and high stress levels are linked to higher cyst prevalence. Maintaining a balanced diet, regular exercise, and stress‑reduction practices can lower overall risk.
Will a cyst affect my chances of getting pregnant?
Typical functional cysts do not impair fertility. Once the cyst resolves and normal ovulation resumes, pregnancy chances return to baseline.
How long should I wait after stopping drospirenone before trying to conceive?
Most women regain normal cycles within 4‑6weeks. A pre‑conception check‑up, including an ultrasound, is advisable to confirm any cyst has cleared.
Are there any non‑hormonal ways to prevent cysts?
Weight management, limiting caffeine, and ensuring adequate vitamin D intake have been associated with fewer functional cysts in some observational studies.

Gregg Deboben
September 23, 2025 AT 06:26Drospirenone is just another Big Pharma scam to keep women hooked on pills while they get cysts and depression. I’ve seen it with my sister-she was on it for 2 years and ended up with a 6cm cyst that needed surgery. No one warned her. The FDA is asleep at the wheel. 🤬
Christopher John Schell
September 23, 2025 AT 23:06Hey everyone, just wanted to say-don’t panic! 😊 Most of these cysts are totally normal and go away on their own. I was on drospirenone for 3 years and had two tiny ones that vanished by the next cycle. You’re not broken, you’re just hormonal. Keep moving, hydrate, and trust your body. You got this! 💪❤️
Felix Alarcón
September 24, 2025 AT 07:05Interesting read. I’m from Mexico and we’ve got a lot of women here on these pills because they’re cheap and effective. But honestly, the cultural attitude here is ‘just deal with it’-no ultrasounds, no questions. Maybe we need more open conversations about this. Also, typo: ‘mineralocorticoid’ is hard to spell. 😅
Lori Rivera
September 24, 2025 AT 16:12The data presented in this article is methodologically sound and aligns with current clinical guidelines. The relative risk increase is statistically insignificant, and the emphasis on lifestyle factors is appropriately prioritized. I would, however, caution against anecdotal extrapolation from individual case reports.
Leif Totusek
September 26, 2025 AT 14:50While the statistical data may suggest minimal risk, the clinical reality for some patients is not so benign. As a physician with over two decades of experience, I have encountered multiple cases of persistent ovarian cysts in patients on drospirenone-containing contraceptives, particularly those with a predisposition to hormonal sensitivity. Caution is warranted.
KAVYA VIJAYAN
September 27, 2025 AT 04:57Okay, so let’s unpack this like a pharmacokinetic puzzle-drospirenone’s anti-mineralocorticoid action reduces edema, which sounds great, but that same mechanism alters the follicular microenvironment by suppressing LH surges too aggressively in some phenotypes, leading to arrested follicular development. In women with subclinical PCOS or low AMH, this isn’t just a ‘cyst’-it’s a sign of disrupted hypothalamic-pituitary-ovarian axis dynamics. And no, switching to levonorgestrel isn’t a magic fix if you’re insulin resistant. You gotta treat the root, not the symptom. Also, vitamin D deficiency is rampant in urban populations-seriously, check your levels before blaming the pill.
Jarid Drake
September 29, 2025 AT 03:51Same here-I was on drospirenone for acne and got a cyst last year. Scared the crap out of me, but my OB said it was just a luteal cyst and to keep taking it. It went away in 2 months. Honestly, I think stress and coffee were bigger culprits than the pill. Just don’t Google symptoms. 😅
Tariq Riaz
September 30, 2025 AT 04:36Study cited: 3.2% vs 2.1%. That’s a 52% relative increase. Not ‘modest.’ Also, 12 trials with n≈9,400? That’s not a meta-analysis, that’s a reanalysis of industry-funded trials. Where’s the independent data? The tone here reads like a pharma whitepaper disguised as medical advice.
Chantel Totten
October 1, 2025 AT 13:30I appreciate the nuance here. I had a cyst while on drospirenone and it was terrifying-but my doctor didn’t panic, and neither did I. We waited. It resolved. I think the fear around this is often worse than the condition itself. Just listen to your body and get checked if something feels off. No need to switch unless it’s recurring.
Guy Knudsen
October 2, 2025 AT 14:56So drospirenone causes cysts? Wow. And I thought the real danger was the government forcing birth control on women to control population. Next they’ll say sunlight causes cancer. Also, who cares about cysts? I’ve got a better question-why do we even need pills? Just have a baby already.
Terrie Doty
October 2, 2025 AT 18:34I’ve been on drospirenone for five years now, and I’ve had two cysts-both during placebo weeks. I didn’t even know I had them until my annual check-up. I’m a quiet person, I don’t like drama, so I just keep taking it. My body feels balanced. I’ve tried other pills, but nothing works as well for my skin and mood. If it ain’t broke, don’t fix it. I’m just glad I didn’t have pain. Some people are so quick to panic. I think it’s more about how we talk about these things than the medicine itself.
George Ramos
October 4, 2025 AT 03:07Ohhhh so THAT’S why my ovaries feel like they’re hosting a rave. 🎉 Drospirenone = synthetic hormone gremlins programmed by Big Pharma to make women bloated and cysty so they’ll buy more pills. They don’t want you healthy-they want you dependent. Ever heard of the ‘Pill-Induced Ovarian Manipulation Initiative’? No? Because it’s classified. My cousin’s OB-GYN got fired for leaking the docs. I’m not paranoid-I’m informed. 🕵️♀️💊
Barney Rix
October 4, 2025 AT 16:11The statistical interpretation presented is misleading. The 95% confidence interval for relative risk includes unity, yet the conclusion implies clinical significance. Furthermore, the exclusion of cyst size distribution and duration data undermines the validity of risk stratification. A more rigorous analysis is required before any clinical recommendation is made.
juliephone bee
October 6, 2025 AT 12:12Wait, so if I have a cyst, do I just… keep taking it? I thought they were supposed to be bad? I’m confused. Also, typo: ‘luteal’ not ‘luteal.’ 😅
Ellen Richards
October 7, 2025 AT 14:29Ugh, I knew it. I’ve been on drospirenone for 4 years and I’ve had 3 cysts. I’m telling you, this pill is poisoning women. My friend’s sister had to get her ovary removed. And now you’re telling me to ‘just wait’? That’s not medical advice-that’s negligence. I’m switching tomorrow. And I’m posting this everywhere.
Renee Zalusky
October 9, 2025 AT 08:49This is beautifully balanced. The interplay between hormonal modulation and follicular dynamics is often oversimplified in patient-facing materials. I particularly appreciate the emphasis on distinguishing functional from pathological cysts-too many patients conflate the two. Also, the note on vitamin D and stress is spot-on; I’ve seen women with chronic cysts improve dramatically after addressing micronutrient deficiencies and sleep hygiene. The pill is a tool, not a villain. Context is everything.
Scott Mcdonald
October 10, 2025 AT 21:20Hey, I’m just wondering-do you think this applies to people who use the patch instead? I’m thinking of switching but I don’t know if the same rules apply. Also, do you think I should get an ultrasound even if I feel fine? Just curious. 😊
Christopher John Schell
October 12, 2025 AT 13:02Hey @Scott Mcdonald, good question! The patch uses the same drospirenone, so the cyst risk is basically the same. If you’re feeling fine, no need for an ultrasound-just keep an eye out for pain or bloating. And if you do switch, give it a few cycles to adjust. You’re not alone in wondering this! 🙌