Digoxin-Amiodarone Dose Adjustment Calculator
Digoxin Dose Adjustment Calculator
This tool helps clinicians adjust digoxin dosing when amiodarone is initiated, based on current guidelines.
Dose Adjustment Recommendation
Important: This adjustment is based on guidelines for initiating amiodarone therapy. Monitor digoxin levels at 72 hours and continue monitoring for 60 days after stopping amiodarone.
When two heart medications are mixed, the stakes are high. Digoxin and amiodarone are both powerful tools for managing irregular heart rhythms and heart failure-but together, they can turn life-saving into life-threatening. This isn’t a theoretical risk. It’s a real, documented, and frequently preventable danger that sends patients to the ICU every year.
Think of digoxin as a precision instrument. It works in tiny doses-just enough to strengthen heart contractions and slow down fast rhythms. But its therapeutic window is razor-thin: blood levels between 0.5 and 0.9 ng/mL are safe. Go above that, and you risk nausea, blurry vision, dangerous heart rhythms, or even death. Amiodarone, on the other hand, is a long-acting antiarrhythmic with a half-life of up to 100 days. It’s effective, but it doesn’t play nice with other drugs. When these two are combined, digoxin levels can spike by 100% or more. And because amiodarone sticks around for months, the danger doesn’t go away quickly-even after you stop taking it.
Why This Interaction Is So Dangerous
Most drug interactions are manageable. A statin and grapefruit juice? Maybe a little higher cholesterol level. But digoxin and amiodarone? This is a high-risk combo for one reason: narrow therapeutic index. That means the difference between the right dose and a toxic dose is small. A little too much digoxin isn’t just uncomfortable-it’s lethal.
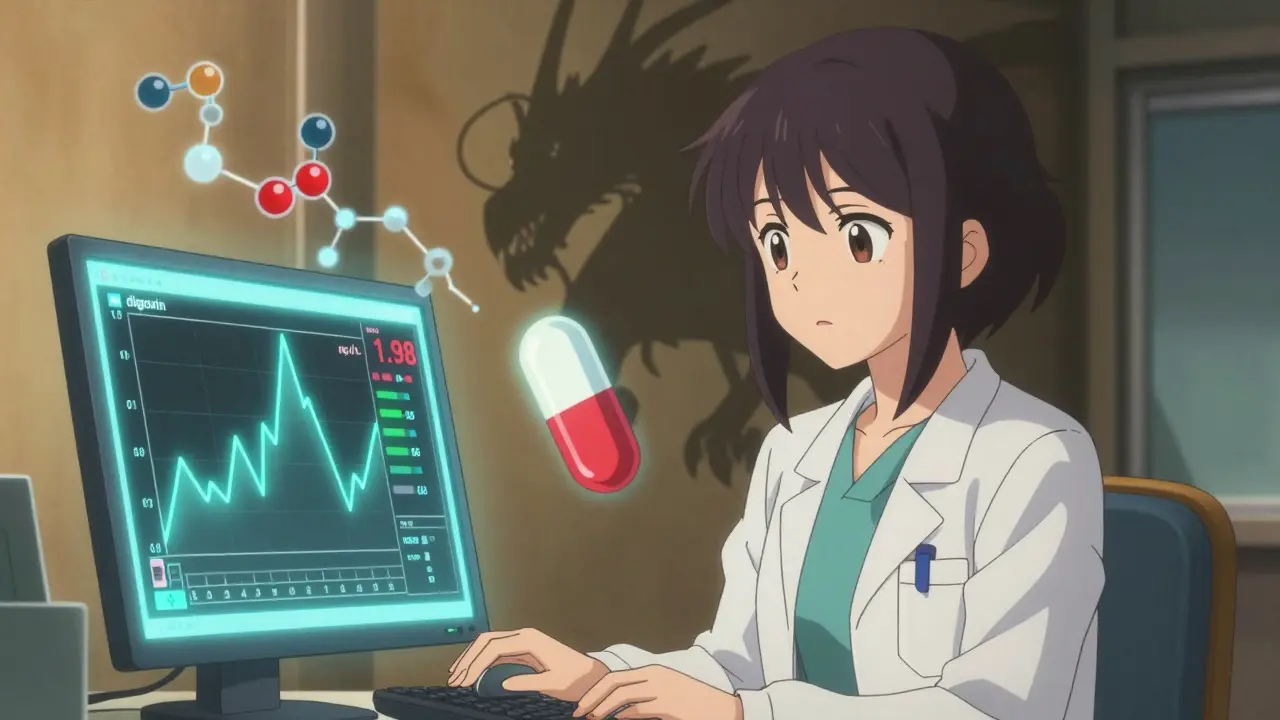
Amiodarone doesn’t just increase digoxin levels-it blocks the body’s ability to clear it. Specifically, it inhibits P-glycoprotein, a transporter protein that normally pushes digoxin out of cells and into the kidneys for elimination. Without this cleanup system, digoxin builds up. Studies show that within days of starting amiodarone, digoxin concentrations can double. One landmark 1984 study found serum digoxin levels jumped from 0.97 ng/mL to 1.98 ng/mL in patients on stable doses. That’s not a fluke. It’s a predictable, repeatable outcome.
And the consequences are real. A 2021 study in Circulation: Arrhythmia and Electrophysiology found patients on both drugs were 2.3 times more likely to be hospitalized for digoxin toxicity than those on other common combinations. Symptoms? Vomiting, confusion, slow heart rate, visual halos, and sudden cardiac arrest. One case report from Massachusetts General Hospital described a 72-year-old woman who developed a potassium level of 6.8 mEq/L-dangerously high-and life-threatening bradycardia after receiving standard digoxin doses alongside new amiodarone therapy. She spent four days in the ICU.
What Happens in the Body
The science behind this interaction is well understood. Amiodarone doesn’t just affect one pathway-it hits multiple.
- It inhibits P-glycoprotein, cutting digoxin clearance by nearly 30%.
- It reduces nonrenal clearance, meaning even if kidneys are working fine, digoxin still builds up.
- Its active metabolite, desethylamiodarone, lingers for weeks after stopping amiodarone and continues to interfere.
This isn’t a short-term problem. The peak interaction doesn’t happen right away. It takes 1 to 2 weeks for digoxin levels to reach their highest point. And because amiodarone has such a long half-life, the risk persists for months-even after you stop taking it. That’s why many clinicians miss it. They check levels after a few days, see them “normal,” and assume it’s safe. But the real danger is coming.
Even more troubling: the interaction isn’t limited to the heart. Elevated digoxin levels can cause kidney dysfunction, electrolyte imbalances, and neurological symptoms. In elderly patients with reduced kidney function, the risk skyrockets. A 2021 analysis in JACC: Heart Failure showed that patients who kept full-dose digoxin while starting amiodarone had a 27% higher chance of dying within 30 days. That’s not a small risk. That’s a crisis waiting to happen.
What Clinicians Are Doing Right-and Wrong
Guidelines have been clear for decades. The 2022 European Heart Rhythm Association Practical Guide says: reduce digoxin by 50% when starting amiodarone. The 2023 ASHP guideline says: check digoxin levels before starting amiodarone, then again at 72 hours. But real-world practice? It’s messy.
A 2022 study across 15 U.S. academic hospitals found only 43.7% of patients had their digoxin dose adjusted when amiodarone was added. In community hospitals? The rate dropped to 31.8%. That means more than half of patients are being put at unnecessary risk.
Why? Time pressure. Lack of awareness. Assumptions. “She’s been on digoxin for years-she’s fine.” But “fine” doesn’t mean safe. One cardiologist on Reddit shared: “I’ve seen three cases of digoxin toxicity from this combo in the past year alone-all in patients over 75 with chronic kidney disease.”
On the flip side, places that implemented protocols saw dramatic improvements. The University of Michigan mandated 50% digoxin dose reduction and mandatory level checks within 72 hours. Result? Toxicity events dropped from 12.3% to 2.1%. The Veterans Health Administration added EHR alerts that trigger when both drugs are prescribed together. Their digoxin toxicity events fell by 41%.
How to Manage This Interaction Correctly
If you’re prescribing or managing a patient on both drugs, here’s what you need to do-no exceptions.
- Check digoxin levels before starting amiodarone. This is your baseline. Don’t skip it.
- Reduce digoxin by 50% at the time you start amiodarone. Do not wait. Do not wait for symptoms. Do not wait for lab results. Start the reduction immediately.
- Recheck digoxin levels at 72 hours. Levels may still be rising. Adjust further if needed.
- For patients with kidney impairment (CrCl <50 mL/min), reduce digoxin by 66% (to one-third of original dose). Their clearance is already compromised. Don’t add to it.
- Monitor for toxicity for at least 60 days after stopping amiodarone. The metabolite sticks around. Symptoms can appear weeks later.
And here’s a critical point: don’t rely on symptoms alone. Nausea, fatigue, and visual changes are late signs. By then, the damage may be done. Regular lab monitoring is non-negotiable.

What About Alternatives?
With so much risk, it’s worth asking: do we even need digoxin when amiodarone is involved?
The 2024 European Society of Cardiology AF guidelines now recommend beta-blockers (like metoprolol) or non-dihydropyridine calcium channel blockers (like diltiazem) as first-line for rate control in atrial fibrillation-especially if amiodarone is planned. These drugs don’t interact with amiodarone in the same way. They’re safer, more predictable, and just as effective for rhythm control in many patients.
Digoxin still has a role-especially in heart failure patients with reduced ejection fraction who don’t respond to other agents. But its use is shrinking. Between 2015 and 2022, digoxin prescriptions in the U.S. dropped by 18%. That’s not just because of new drugs. It’s because doctors are learning the hard way that this interaction isn’t worth the risk.
The Bottom Line
This interaction isn’t rare. It’s common. With over 1.2 million Americans on both drugs, it’s happening in clinics and hospitals every day. And it’s preventable.
The fix isn’t complicated. Reduce the digoxin dose. Check the levels. Monitor for weeks. Educate the patient. It’s not about being overly cautious. It’s about being clinically responsible.
When you combine two drugs with narrow therapeutic indices, you’re playing with fire. The data is clear. The guidelines are clear. The consequences of ignoring them are not. Don’t wait for a patient to crash before you act. Do the math. Reduce the dose. Save a life.

Jasmine Yule
December 30, 2025 AT 08:53This is why I hate when doctors just prescribe without checking interactions. My grandma almost died from this exact combo. They didn't adjust her digoxin and she started seeing halos around lights. Took three days to figure out what was wrong. Don't be that doctor.
Greg Quinn
December 31, 2025 AT 12:35It's wild how a drug with a half-life of 100 days can quietly sabotage another one for months. We treat meds like they're light switches-on or off-but amiodarone is more like a slow-burning fuse. The real tragedy is how often this gets missed because no one thinks to look past the first week.
Lisa Dore
January 1, 2026 AT 10:40Love this breakdown. Seriously. As a nurse, I’ve seen too many elderly patients get shuffled through the system without anyone connecting the dots. We need more posts like this-clear, data-backed, and urgent. Sharing this with my whole unit tomorrow.
Henriette Barrows
January 2, 2026 AT 20:55My dad’s on both meds and I’ve been monitoring his labs like a hawk. The 50% dose reduction saved his life. He’s 82, has CKD, and we cut his digoxin down hard. No symptoms since. Just wanted to say thank you for putting this out there. People need to know.
Alex Ronald
January 4, 2026 AT 12:21Just a quick note: if you’re using amiodarone long-term, don’t forget to check thyroid function too. It’s not just digoxin-it’s a whole cascade of side effects. One less thing to miss.
Teresa Rodriguez leon
January 6, 2026 AT 02:17This is why I don’t trust modern medicine. They just throw drugs at people and hope something sticks. My cousin ended up in the ICU and no one even told her family about the risk. Now she’s on dialysis. Great job, doctors.
Manan Pandya
January 6, 2026 AT 04:39Excellent summary. In India, we see this frequently in cardiac units where polypharmacy is common and monitoring resources are limited. The 50% reduction rule must be institutionalized-not left to individual vigilance. Protocols save lives.
Aliza Efraimov
January 7, 2026 AT 02:10Y’all are underestimating how terrifying this interaction is. I had a patient go into torsades de pointes at 3 a.m. because his digoxin level was 2.8 ng/mL. He was on amiodarone for two weeks. No one adjusted the dose. He coded. We brought him back. He’s alive. But he’ll never forget it. And neither will I. This isn’t theory. It’s trauma.
Nisha Marwaha
January 7, 2026 AT 15:40The pharmacokinetic interplay between amiodarone and digoxin is mediated by P-glycoprotein inhibition, which impairs renal and nonrenal clearance pathways. The active metabolite, desethylamiodarone, exhibits prolonged half-life kinetics, thereby sustaining the interaction beyond the cessation of amiodarone administration. This necessitates vigilant therapeutic drug monitoring over a 60-day window post-discontinuation.
Paige Shipe
January 9, 2026 AT 13:00I think you’re overreacting. My uncle took both for years and never had a problem. Maybe people just need to be more careful instead of making everything sound like a disaster. Also, digoxin is cheap and works. Why replace it?
Amy Cannon
January 10, 2026 AT 08:39It is with the utmost gravity and solemnity that I address the profound implications of this pharmaceutical interaction, which, if left unattended, may precipitate catastrophic outcomes in the geriatric population, particularly those with compromised renal function, wherein the pharmacodynamic synergy between amiodarone and digoxin may yield a lethal confluence of bioavailability dysregulation and delayed toxin accumulation, thereby demanding not merely clinical caution, but systemic, protocol-driven intervention across all levels of care delivery.
Himanshu Singh
January 12, 2026 AT 06:02Good post! I work in a rural clinic and we don’t always have quick lab access. But now I’m making sure to reduce digoxin by half right away, even if we can’t check levels right away. Better safe than sorry. Thanks for the reminder!