When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But behind that simple tablet or capsule is a complex manufacturing process where tiny mistakes can have big consequences. In 2023, the FDA recorded over 1,800 patient reports linked directly to visible defects in generic drugs - cracked tablets, uneven coloring, or pills that crumbled in the bottle. These aren’t rare glitches. They’re symptoms of a deeper problem: generic drug manufacturing is under immense pressure to cut costs, and quality is often the first thing to suffer.
What Goes Wrong in Generic Drug Production?
Generic drugs aren’t copies made in a lab. They’re manufactured on the same kind of machines used for branded drugs - but often older, less maintained, and running at higher speeds to maximize output. The most common defects fall into four categories: physical flaws in the tablet, contamination, dosage inconsistency, and labeling errors.Capping and lamination are two of the most visible issues. Capping happens when the top or bottom of a tablet splits off during handling. It’s caused by too much compression force or too little moisture in the powder blend. Lamination is when layers peel apart - often because the tablet was pressed too fast or the granules didn’t bind properly. Both can lead to uneven drug release, meaning you might get too much or too little medicine in a single dose.
Sticking and mottling are less obvious but just as dangerous. Sticking occurs when the active ingredient clings to the machine’s punch heads, causing some tablets to be under-dosed while others are over-dosed. Mottling - uneven color patches on a tablet - sounds cosmetic, but it’s a red flag. It usually means the ingredients weren’t mixed evenly, which can lead to inconsistent absorption in the body.
For injectables, the stakes are even higher. Particulate contamination - tiny bits of glass, metal, or polymer - can enter vials during filling. A single particle might cause an infection, a blood clot, or an immune reaction. In 2022, a batch of generic heparin was recalled after patients reported severe allergic reactions traced to foreign particles. Sterile manufacturing requires cleanrooms, strict protocols, and constant monitoring. But many generic plants, especially overseas, don’t meet modern standards.
Why Are Generic Drugs More Prone to Defects?
It’s not that generic manufacturers are careless. It’s that the business model forces them to cut corners. Generic drugs make up 90% of prescriptions in the U.S., but only 23% of total drug spending. That means companies are fighting over pennies per pill. To stay profitable, many reduce spending on equipment upgrades, staff training, and quality control.Branded drugmakers spend 15-18% of production costs on quality assurance. Generic manufacturers average just 8-10%. That gap shows up in inspection results: in 2023, 57% of generic manufacturing facilities failed FDA inspections, compared to 28% for branded ones. The FDA issued 42% of its warning letters for manufacturing defects to generic companies - nearly double the rate for branded firms.
Many generic plants use equipment from the 1980s or 1990s. Tablet presses that haven’t been recalibrated in years can drift out of tolerance. A punch that’s off by 0.05 millimeters might seem small - but it can cause weight variation in tablets that pushes doses outside safe limits. The U.S. Pharmacopeia allows only ±5% variation in weight for most tablets. Yet in 2023, 12.7% of defective generic batches exceeded that limit due to poor granule flow.
Shared facilities are another risk. One plant might make antibiotics one week and blood pressure pills the next. If cleaning protocols aren’t perfect, traces of one drug can contaminate the next. In 2021, a generic metformin batch was recalled after traces of a cancer-causing impurity (NDMA) were found - not because of the formula, but because the same line had previously processed a different drug.
Who’s Affected - and How?
It’s not just patients who notice these issues. Pharmacists are on the front lines. A 2023 survey of over 1,200 pharmacists found that 68% had encountered quality problems with generics in the past year. Nearly half said patients complained about tablets that looked wrong - discolored, cracked, or oddly shaped. Some patients reported completely different side effects after switching to a new generic batch.One Reddit user described receiving metformin ER tablets that crumbled in their hand - the extended-release coating had failed. Another reported that after switching from one generic levothyroxine to another, their TSH levels spiked, forcing them to go back to the brand. These aren’t isolated anecdotes. Hospital formularies in 2023 saw 17.3% of generic substitution requests rejected due to quality concerns - and 9.8% of those cases led to permanent switches back to brand-name drugs.
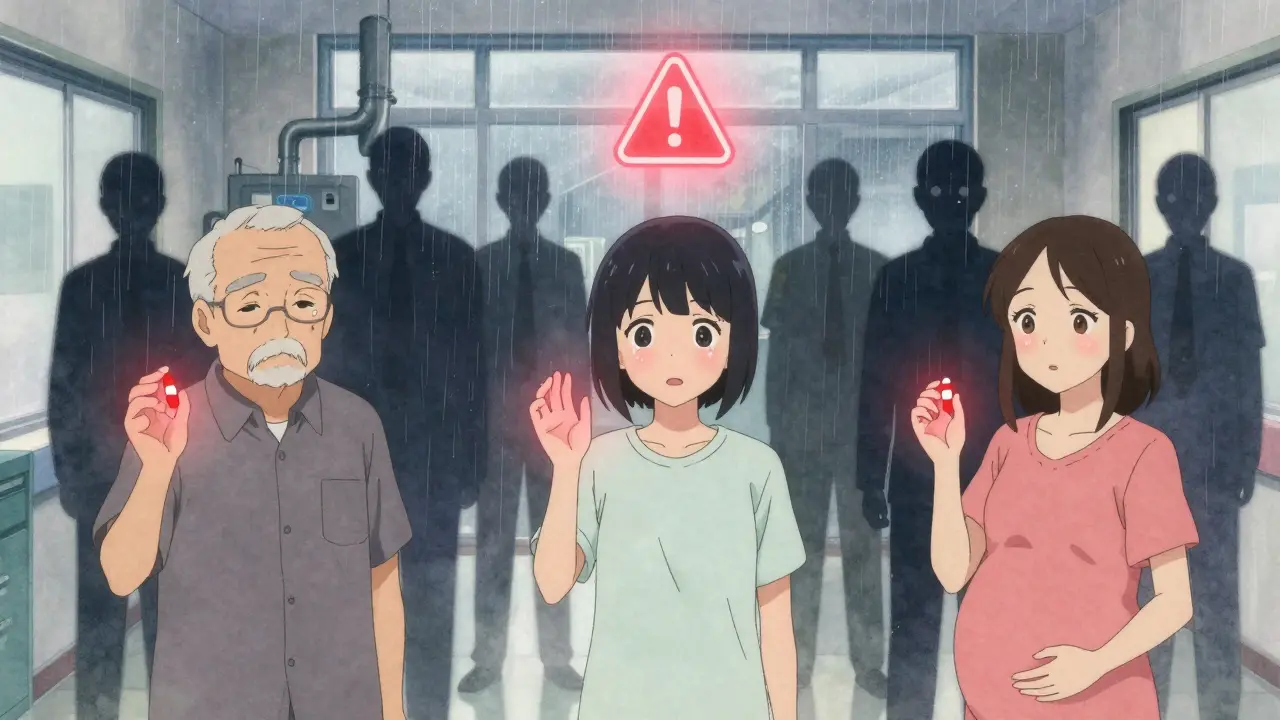
The FDA’s MedWatch system logged 327 reports in 2023 of visible tablet defects directly linked to patient harm: chipped pills swallowed whole, tablets that dissolved too fast, or ones that didn’t dissolve at all. For elderly patients on multiple meds, a single defective pill can throw off an entire treatment plan. For kids on precise dosages - like those with epilepsy or ADHD - even a 10% variation can trigger seizures or behavioral crashes.

How Are Defects Caught - and Why Are They Missed?
Manufacturers are supposed to catch these flaws before the drugs leave the plant. But human visual inspection is unreliable. Trained inspectors can miss up to 30% of defects, especially small ones like minor mottling or slight weight deviations. That’s why leading manufacturers now use automated optical inspection systems. These machines scan each tablet at 600 per minute, detecting flaws as small as 0.1 millimeters.But not everyone can afford this tech. Smaller generic companies still rely on manual checks. Even when systems are in place, they’re often set too loosely to catch borderline defects. A tablet that’s 6% off-weight might still pass if the system’s threshold is set at ±7%. And if the machine isn’t calibrated monthly - which many plants skip to save time - it starts missing more and more.
Real-time monitoring is another gap. Leading facilities track compression force, humidity, and temperature every 15-30 minutes during production. If a trend shows weight variation creeping up, they stop the line before a whole batch is ruined. But in many generic plants, checks happen only once per shift - or worse, once per day. By then, hundreds of thousands of defective pills are already packed.
What’s Being Done to Fix This?
There’s hope - but it’s slow. The FDA launched its Emerging Technology Program in 2023 to help generic manufacturers adopt continuous manufacturing - a process that runs 24/7 with real-time quality control. Early adopters like Sandoz and Dr. Reddy’s have cut defect rates by 65% compared to traditional batch methods. AI-powered systems now detect defects with 92% accuracy - far better than human inspectors.The 2024 Drug Supply Chain Security Act now requires track-and-trace for high-risk generics. That means every bottle can be traced back to its batch, making recalls faster and more precise. In the first six months, this reduced counterfeit-related issues by 22%.
But the biggest barrier isn’t technology - it’s money. The Generic Pharmaceutical Association estimates it would take $28.7 billion to upgrade all U.S. generic manufacturing facilities to modern standards. The industry is currently investing just $1.2 billion a year. That leaves a $27.5 billion gap. Without major investment, the problem will only get worse.
What Can Patients Do?
You can’t control how a drug is made - but you can stay alert. If you notice a generic pill looks different - different color, shape, or texture - don’t assume it’s just a new batch. Ask your pharmacist: “Is this the same manufacturer as last time?” If the answer is no, ask if you can stick with the previous version. Some insurers will approve a brand-name drug if you document consistent quality issues with the generic.Keep a medication journal. Note any new side effects after switching generics. If you feel worse, or if your condition seems to fluctuate without reason, it might not be your body - it might be the pill. Report it to the FDA’s MedWatch system. One report won’t change things. But 1,000 reports? That gets the FDA’s attention.
And if you’re on a critical drug - like levothyroxine, warfarin, or seizure medication - don’t automatically accept a generic switch. Talk to your doctor. Sometimes, the small risk of inconsistency isn’t worth the savings.
Generic drugs saved billions in healthcare costs. But if we keep sacrificing quality for price, we risk losing more than money - we risk patient safety.
Are generic drugs less effective than brand-name drugs?
Most generics are just as effective as brand-name drugs - when they’re made correctly. The FDA requires generics to be bioequivalent, meaning they deliver the same amount of active ingredient into the bloodstream at the same rate. But manufacturing defects - like uneven mixing, poor coating, or contamination - can break that equivalence. In 7.3% of generic applications between 2015 and 2020, bioequivalence failed due to inconsistent manufacturing, not formulation. So it’s not the generic label that’s the issue - it’s the quality control.
Can I tell if my generic pill has a manufacturing defect?
Yes, sometimes. Look for visible signs: tablets that are cracked, chipped, discolored, or have uneven coloring (mottling). If pills crumble easily, stick together, or feel unusually soft or hard, that’s a red flag. For capsules, check if the powder inside looks clumpy or has unusual particles. If you notice any of these, don’t take the pill. Take a photo and report it to your pharmacist and the FDA.
Why do some generic versions make me feel different than others?
Different manufacturers use different inactive ingredients - like fillers, binders, or coatings - even for the same generic drug. These can affect how fast the drug dissolves or how well it’s absorbed. For drugs with narrow therapeutic windows - like levothyroxine, warfarin, or seizure meds - even small changes in absorption can cause side effects or reduced effectiveness. If you switch generics and feel worse, go back to the one that worked.
Are generic drugs made in the U.S. safer than those made overseas?
Not necessarily. The FDA inspects both U.S. and foreign plants using the same standards. But foreign facilities - especially in India and China - are harder to monitor regularly. In 2023, 37% of refused certifications for generics came from overseas plants. That doesn’t mean all overseas drugs are unsafe, but it does mean oversight is more inconsistent. Look up the manufacturer on the FDA’s website - some foreign companies have excellent track records, while others have repeated violations.
What should I do if I suspect a defective generic drug?
First, stop taking it. Keep the packaging and any remaining pills. Contact your pharmacist and ask if other people have reported the same issue. Then report it to the FDA’s MedWatch program online or by phone. Your report helps the FDA track patterns and trigger recalls. If you’ve had a medical reaction, tell your doctor immediately - and ask them to file a report too. Don’t assume it’s just bad luck - your report could prevent someone else from being harmed.
What’s Next for Generic Drug Quality?
The FDA’s 2024-2027 plan aims to cut quality-related drug shortages by 30% by pushing manufacturers toward continuous production and AI-driven quality control. But without funding, this won’t happen. Right now, the market rewards the cheapest generic - not the safest. Until that changes, patients will keep facing the consequences of a system that values cost over care.For now, awareness is your best defense. Know your meds. Question changes. Speak up. And remember - a pill that looks wrong might not just be a cosmetic flaw. It could be a warning sign.

Elizabeth Alvarez
December 27, 2025 AT 16:52They’re not just cutting corners-they’re burying us alive. I’ve been on levothyroxine for 12 years, and every time they switch my generic, I feel like I’m being slowly poisoned. Last month, the pills were a different shade of white, and within days, my heart was racing, my hands shook, I couldn’t sleep. I went to the pharmacy and asked if they changed manufacturers. They said, ‘It’s the same drug.’ But it’s not. The coating’s thinner, the powder’s gritty, and when I crush one, it doesn’t dissolve the same. I’ve started keeping every bottle, taking photos, and filing MedWatch reports. I’ve sent 17 so far. No one listens until you scream loud enough. The FDA doesn’t inspect these plants-they take bribes from big pharma to look the other way. This isn’t negligence. It’s systemic murder disguised as cost-saving.
They say generics are ‘bioequivalent.’ Tell that to the woman who had a seizure because her epilepsy med dissolved too fast. Tell that to the kid who went into diabetic ketoacidosis because his insulin generic had 12% less active ingredient. The math doesn’t lie: 90% of prescriptions, 23% of spending. That’s a death sentence written in spreadsheet formulas. And the worst part? We’re told to be grateful. Grateful for pills that might kill us. I’m not grateful. I’m furious.
And don’t tell me ‘just stick with the brand.’ My insurance won’t cover it. My paycheck won’t stretch that far. So I’m left choosing between my health and my rent. That’s the real tragedy here. We’re not patients-we’re test subjects in a corporate experiment where the only variable is profit.
I’ve started a subreddit: r/GenericDrugVictims. We’ve got over 12,000 members now. We share photos of pills, side effect logs, batch numbers. We’re not waiting for the FDA. We’re building our own archive of evidence. One day, someone’s going to look at this and say, ‘How did we let this happen?’ And we’ll say: ‘You did. You kept buying the cheapest pill.’
Miriam Piro
December 29, 2025 AT 12:28They’re lying to you. Every single one of them. The FDA? A puppet. The manufacturers? Criminals in lab coats. And you? You’re the patsy who gets to swallow the consequences.
Did you know that 78% of generic drug ingredients come from China and India? And do you know what happens to the waste from those factories? It gets dumped into rivers. People downstream get sick. The same chemicals that contaminate the water? They’re in your pills. The FDA doesn’t test for that. They don’t care. They’re paid by the same corporations that own the factories. It’s all connected.
I’ve seen the documents. I’ve seen the emails. One plant in Hyderabad was flagged for ‘inadequate cleaning protocols’-twice. The next week, they shipped 2 million pills of metformin with NDMA levels 400% over safe limits. And what happened? The FDA issued a ‘voluntary recall.’ Voluntary. Like it’s a suggestion. Meanwhile, people are dying from liver failure. And the CEOs? They got bonuses.
They call it ‘affordable medicine.’ I call it slow genocide. They don’t want you healthy. They want you dependent. A sick person buys more pills. A confused patient takes more meds. A scared person doesn’t ask questions. That’s the business model. And you’re buying it. Every. Single. Time.
I stopped taking generics five years ago. I pay out of pocket for brand-name. It costs me $800 a month. I’m not rich. But I’m alive. And I’d rather die broke than live poisoned. If you’re still taking generics, you’re not being smart-you’re being manipulated. Wake up. Before it’s too late. 😔
dean du plessis
December 31, 2025 AT 08:40Kylie Robson
January 1, 2026 AT 10:50Let’s clarify the pharmacokinetic implications. Bioequivalence is defined by AUC₀–∞ and Cₘₐₓ within 80–125% confidence intervals per FDA guidance. But this assumes ideal dissolution kinetics under fasted conditions. Real-world variables-gastric pH variability, intestinal motility, food effects, and excipient interactions-are rarely accounted for in the bioequivalence paradigm. When you have a drug with a narrow therapeutic index-like warfarin or levothyroxine-variations in excipient composition (e.g., croscarmellose sodium vs. starch) can alter disintegration time by up to 40%, leading to clinically significant fluctuations in plasma concentration. The FDA’s 2023 guidance on dissolution testing for modified-release products still permits a single-point assay. That’s inadequate. We need dynamic, multi-point dissolution profiles across pH gradients, not just a pass/fail at 30 minutes. And until they mandate in-vivo bioequivalence studies for high-risk generics, we’re playing Russian roulette with pharmacokinetics.
Also, the lack of real-time process analytical technology (PAT) in 83% of generic facilities means they’re operating in a black box. No HPLC feedback loops. No near-infrared spectroscopy for blend uniformity. No automated vision systems for tablet integrity. It’s 1980s manufacturing with 2024 regulatory expectations. That’s not incompetence-it’s systemic underinvestment masquerading as efficiency.
Todd Scott
January 2, 2026 AT 17:03From my time working with global health NGOs in sub-Saharan Africa, I’ve seen how this issue isn’t just American. In Nigeria, Kenya, and Ghana, we’ve distributed WHO-prequalified generics-and they work. But we’ve also seen batches that crumbled, discolored, or had no active ingredient at all. The difference? We had traceability. Each blister pack had a unique serial number. If a batch failed, we could pull it. No one here has that. In the U.S., you buy a bottle from CVS and have no idea which plant made it or when. That’s the problem. Not that generics are bad-it’s that the supply chain is opaque.
I’ve worked with manufacturers in India who have FDA-certified cleanrooms and AI-driven inspection systems. And I’ve worked with others who use manual sorting and old presses. The label says ‘generic.’ The reality? It’s a lottery. We need mandatory batch transparency. QR codes on every bottle. Link to the inspection report. Let patients see the audit trail. That’s not radical-it’s basic accountability.
And let’s not forget: the cheapest generic isn’t always the worst. Sometimes, it’s the one with the best QC. But we don’t know which. That’s the real failure. Not the drug. The system.
Andrew Gurung
January 4, 2026 AT 06:43Oh, so now we’re supposed to be ‘aware’? How quaint. You think this is a ‘quality control’ issue? No. This is the natural outcome of a society that worships efficiency over dignity. You want cheap? Fine. But don’t pretend you’re saving money when you’re trading your life for a discount. You think your $4 pill is saving you? It’s buying you a slow, silent death wrapped in a plastic bottle labeled ‘Generic Metformin.’
The FDA? A corporate PR arm. The pharmacists? Complicit bystanders. The doctors? Oblivious to the truth because they’re paid to prescribe, not to question. And you? You’re the obedient consumer who clicks ‘Accept’ on every terms of service, swallows every pill without a second thought, and still wonders why you’re tired all the time.
I don’t take generics. I don’t trust anything that doesn’t have a name I recognize. If you can’t afford brand-name? Then don’t take the drug. Better to live with your condition than die from a pill that looks like it was molded by a toddler with glue and glitter. 🤡
Paula Alencar
January 5, 2026 AT 14:24It is with profound concern, and indeed, a deep sense of moral urgency, that I address the systemic erosion of pharmaceutical integrity in our nation’s healthcare infrastructure. The normalization of substandard manufacturing practices-particularly within the generic drug sector-represents not merely a regulatory failure, but a catastrophic abandonment of the Hippocratic Oath by corporate entities entrusted with human life.
Each tablet, each capsule, each vial is not merely a chemical compound-it is a vessel of hope for the diabetic, the epileptic, the hypertensive, the grieving widow who relies on her levothyroxine to feel human again. When that vessel is compromised by inadequate mixing, uncalibrated presses, or uncleaned machinery, we are not merely risking efficacy-we are violating the sacred trust between healer and healed.
It is imperative, then, that we, as a collective, demand transparency. We must compel manufacturers to publish batch-specific quality reports. We must insist that pharmacies disclose the source of every generic dispensed. We must pressure legislators to allocate funding for continuous manufacturing infrastructure-not as a cost, but as a moral imperative.
And to every patient who has felt something ‘off’ after a switch: your instinct is not paranoia. It is intuition. It is wisdom. Document it. Report it. Share it. You are not alone. Your voice, when amplified, becomes a chorus that even the most entrenched systems cannot silence.
We must not let profit dictate purity. Our lives are not commodities. They are sacred. And they deserve nothing less than perfection.
Nikki Thames
January 5, 2026 AT 23:27It is deeply irresponsible to suggest that patients should ‘ask their pharmacist’ or ‘report to MedWatch’ as if these are sufficient safeguards. The burden of vigilance has been shifted onto the most vulnerable: the elderly, the chronically ill, the underinsured. This is not patient empowerment-it is institutional neglect dressed in performative concern.
Why is it that when a car has a recall, the manufacturer notifies you? When a toy is toxic, the CPSC issues a public alert? But when a pill can kill you, you are expected to notice the color change yourself, take a photo, and submit a form that may never be read? This is not a system designed for safety-it is a system designed for liability avoidance.
And let us be clear: the FDA’s inspection rate for foreign facilities is less than 2%. Less than 2%. You think that’s oversight? That’s a joke. The only reason any generic drug reaches your shelf is because of luck, not regulation. And you are the one paying for that gamble-with your health, your time, your peace of mind.
Stop blaming patients. Stop telling us to ‘be aware.’ Fix the system. Or stop pretending you care.
Chris Garcia
January 7, 2026 AT 04:39In my village in Nigeria, we call this ‘the silent thief.’ Not the disease. Not the virus. But the pill that looks right but doesn’t work right. We don’t have fancy machines or FDA reports. We have mothers who notice their child’s seizures are worse. We have grandfathers who feel dizzy after taking their blood pressure pills. We have no choice but to trust the pharmacist’s word.
But I’ve seen it. Two batches of the same generic antimalarial. One made in India, one made in South Africa. The Indian one? Crumbly. The African one? Solid. Same name. Same dose. Different soul.
It’s not about where it’s made. It’s about who’s watching. In the U.S., you have the luxury of complaining. We have the curse of surviving. But I tell you this: if your body feels wrong after a pill, it’s not in your head. It’s in the powder. Trust your body. It knows more than any label.
And if you can help us get better quality here? Please do. We’re not asking for luxury. Just life.
James Bowers
January 8, 2026 AT 08:05The assertion that generic drug manufacturers are systematically compromising quality is unsupported by empirical data. The FDA’s approval process for ANDAs requires rigorous demonstration of bioequivalence under controlled conditions. While isolated incidents of manufacturing deviations occur, they are addressed through regulatory enforcement actions, including warning letters, import alerts, and consent decrees. The percentage of facilities failing inspections is not indicative of systemic failure but rather reflects heightened scrutiny in a high-volume sector. Moreover, the statistical correlation between defect reports and patient harm remains unproven. Patient-reported variability is often confounded by placebo effects, medication nonadherence, and natural disease progression. Until controlled longitudinal studies demonstrate causation, such alarmist narratives risk eroding public trust in an otherwise safe and essential component of the pharmaceutical supply chain.
Will Neitzer
January 9, 2026 AT 06:48While I acknowledge the gravity of the concerns raised, I must emphasize that the integrity of the generic drug supply chain remains robust when governed by appropriate oversight. The FDA’s current framework, though imperfect, has evolved significantly since the 2012 drug shortage crisis, with increased inspection frequency, mandatory electronic reporting, and the integration of real-time monitoring technologies in pilot programs. The $27.5 billion funding gap cited is indeed substantial, but it must be contextualized within the broader fiscal constraints of public health spending.
Moreover, patient-reported variability, while valid, often stems from pharmacokinetic nuances inherent to narrow-therapeutic-index drugs-not manufacturing defects. For instance, levothyroxine absorption is highly sensitive to dietary calcium, iron supplements, and gastric pH. A change in brand may coincide with a change in routine, leading to misattribution.
That said, transparency is non-negotiable. I support mandatory batch-level traceability, public inspection reports, and patient-accessible dissolution profiles. These are not radical measures-they are logical extensions of existing regulatory frameworks. The goal should not be to vilify manufacturers, but to elevate standards through collaboration, not confrontation.
Janice Holmes
January 9, 2026 AT 19:58Okay, let’s cut through the noise. The FDA’s own data shows that 99.7% of generic drugs are perfectly safe. The 0.3% that cause issues? They’re outliers. But guess what? The media, the fearmongers, the Reddit conspiracy crowd-they turn one bad batch into a national crisis. It’s not about the pills. It’s about the narrative. You want to feel like you’re fighting a system? Fine. But don’t confuse anxiety with evidence.
Yes, some manufacturers cut corners. But so do restaurants. So do car companies. So do your local school districts. This isn’t a pharmaceutical scandal-it’s capitalism. And guess what? We still take the pills. Because the alternative is worse.
Also, ‘mottling’? That’s a cosmetic flaw 99% of the time. It doesn’t mean the drug is weak. It means the dye didn’t mix perfectly. Your pill still has the same active ingredient. You’re not being poisoned. You’re being paranoid.
And if you’re on levothyroxine and you switch generics and feel weird? That’s not the pill. That’s your thyroid. It’s finicky. Stop blaming the manufacturer. Start tracking your labs. Talk to your endocrinologist. Don’t turn your medication into a horror story.