Anticholinergic Burden Calculator
Medication Risk Assessment
This calculator helps you assess your risk of anticholinergic side effects from medications. Based on the University of Washington's Anticholinergic Cognitive Burden (ACB) scale.
Your Medication Risk Assessment
Total ACB Score:
Recommended Actions
Combining antihistamines with other sedating medications can be dangerous-even deadly. If you're taking something for sleep, anxiety, pain, or allergies, you might be at risk without even realizing it. This isn't just a theoretical concern. Every year, over 300,000 people in the U.S. end up in the emergency room because of these kinds of drug interactions. And the most common culprit? Over-the-counter antihistamines like Benadryl.
Why Some Antihistamines Are Riskier Than Others
Not all antihistamines are the same. There are two main types: first-generation and second-generation. The difference isn't just about how well they work for allergies-it's about how they affect your brain and body. First-generation antihistamines like diphenhydramine (Benadryl), hydroxyzine, and promethazine are designed to cross the blood-brain barrier. That’s why they make you sleepy. But that same property makes them dangerous when mixed with other drugs that slow down your nervous system. These drugs also have strong anticholinergic effects, meaning they block acetylcholine, a key brain chemical. On the Anticholinergic Cognitive Burden (ACB) scale, diphenhydramine scores a 3-the highest level of risk. That’s worse than many prescription sedatives. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) were made to avoid the brain. They barely cross the blood-brain barrier, thanks to special transporters that push them out. As a result, they don’t cause drowsiness in most people. Their ACB score is 0 or 1, meaning they’re far safer to take with other medications.What Medications Are Most Dangerous to Mix With Antihistamines?
Here’s where things get risky. Mixing first-generation antihistamines with any of these can lead to serious side effects:- Benzodiazepines (like Xanax, Valium, Ativan): These are used for anxiety and sleep. When combined with diphenhydramine, studies show sedation increases by up to 42%. One study found patients couldn’t perform simple tasks after taking both.
- Opioids (like oxycodone, hydrocodone, codeine): These slow breathing. Add diphenhydramine, and the risk of respiratory failure jumps from 1.5% to 8.7%. The CDC lists this as a top cause of accidental overdose.
- Alcohol: Even one drink with 25mg of Benadryl can cause blackouts, extreme dizziness, or loss of coordination. Users on Reddit and WebMD report hospital visits after just one night of mixing them.
- Sleep aids (like zolpidem/Ambien): These are already CNS depressants. Adding diphenhydramine multiplies the effect, increasing fall risk and confusion, especially in older adults.
- Antidepressants (like trazodone, amitriptyline): Many have anticholinergic properties. Layering them with Benadryl can lead to delirium, rapid heartbeat, or urinary retention.
- Cimetidine (Tagamet): This older heartburn drug blocks liver enzymes that break down antihistamines. That means diphenhydramine stays in your system longer, increasing toxicity.
Who’s at the Highest Risk?
Older adults are the most vulnerable. As people age, their liver and kidneys clear drugs more slowly. A 70-year-old taking diphenhydramine may have 50-70% higher drug levels than a 30-year-old. That’s why the American Geriatrics Society put first-generation antihistamines on their Beers Criteria list of medications to avoid in seniors. But it’s not just age. People taking three or more medications with anticholinergic effects are at extreme risk. A 2021 JAMA study found that combining diphenhydramine with oxybutynin (for overactive bladder) increased delirium risk by 54%. Another study linked long-term use of high-ACB drugs to a 54% higher chance of developing dementia. Even young people aren’t safe. A Reddit thread with nearly 500 upvotes told the story of someone who nearly died after mixing Benadryl with Xanax. Others reported passing out after one drink and one pill. These aren’t rare cases-they’re common enough that GoodRx gives diphenhydramine a 1.8 out of 5 stars for safety.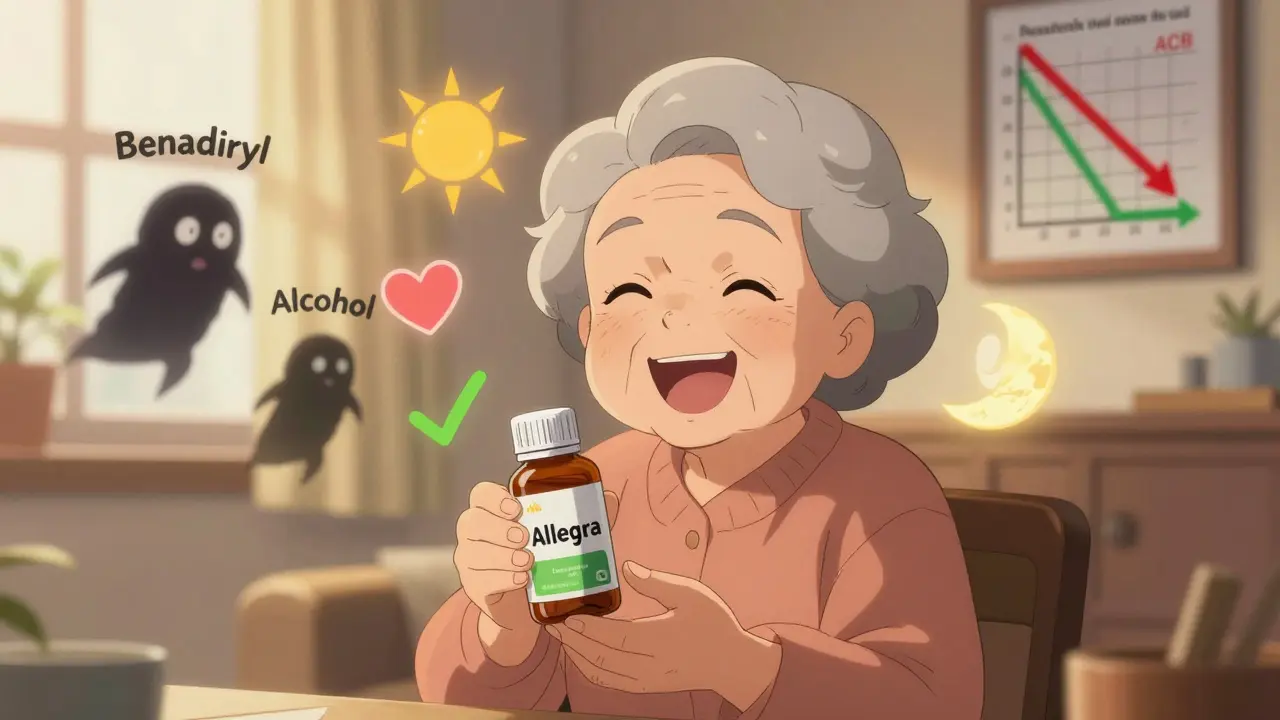
What About ‘Nondrowsy’ Antihistamines?
Loratadine, cetirizine, and fexofenadine are called “nondrowsy,” but that doesn’t mean zero risk. Cetirizine still has an ACB score of 1, and while it rarely causes drowsiness, it can still interact with strong sedatives like opioids or benzodiazepines. If you’re taking multiple CNS depressants, even a low-risk antihistamine isn’t completely safe. The real winner is fexofenadine (Allegra). It has no anticholinergic activity, doesn’t affect liver enzymes, and shows no interaction with benzodiazepines in clinical trials. In user reviews, Allegra gets 4.3 out of 5 stars on Amazon, with people praising it for “no drowsiness even with my other meds.” Benadryl, by contrast, gets 2.9 out of 5, with 68% of negative reviews citing dangerous drowsiness.What Should You Do Instead?
If you’re using diphenhydramine for allergies, switch to a second-generation option. Claritin, Zyrtec, or Allegra work just as well for hay fever, hives, and runny nose-with none of the brain fog or danger. If you’re using it for sleep, there are better choices. Melatonin, magnesium, or cognitive behavioral therapy for insomnia (CBT-I) are safer long-term solutions. Even low-dose doxylamine (Unisom) is slightly less risky than diphenhydramine, but still not ideal for regular use. For motion sickness, dimenhydrinate (Dramamine) is still a valid use case-but only for short trips. Don’t take it daily. For chronic nausea or vertigo, talk to your doctor about alternatives like meclizine, which has a lower anticholinergic burden.How to Check Your Medication Risk
You don’t need to be a pharmacist to protect yourself. Here’s how to check your risk:- Make a list of every medication you take, including OTC pills, supplements, and alcohol.
- Look up each drug’s ACB score. You can use the University of Washington’s free Anticholinergic Burden Calculator.
- Add up the scores. If your total is 3 or higher, you’re at increased risk for confusion, falls, and cognitive decline.
- Ask your pharmacist or doctor to review your list. Many pharmacies now flag high-risk combinations automatically.
- If you’re over 65 or take 5+ medications, ask if you can switch to second-generation antihistamines.
What’s Changing in 2025?
The tide is turning. Since 2018, sales of first-generation antihistamines have dropped 12.7% each year. In 2023, 83% of the U.S. OTC antihistamine market was second-generation drugs. The FDA now requires bold warnings on Benadryl packaging: “May cause severe drowsiness when combined with alcohol, opioids, or sleep medications.” Newer antihistamines like bilastine and levocetirizine are being developed to eliminate off-target effects entirely. A 2023 study showed bilastine had no interaction with lorazepam-even at double the normal dose. That’s the future: effective allergy relief without sedation or danger. Meanwhile, hospitals like Kaiser Permanente have automated systems that alert doctors when a patient is prescribed a dangerous combo. These systems cut antihistamine-related ER visits by 34% between 2020 and 2022.Bottom Line: Don’t Guess. Check.
If you’re taking any sedating medication-whether it’s a prescription, OTC pill, or just a nightly drink-don’t assume Benadryl is safe. The risks are real, well-documented, and preventable. Most people don’t know their allergy medicine could be making their anxiety or pain meds more dangerous. Switch to a second-generation antihistamine. Talk to your pharmacist. Use a free tool to check your drug list. Your brain, your breathing, and your safety depend on it.Can I take Benadryl with alcohol?
No. Mixing Benadryl (diphenhydramine) with alcohol can cause extreme drowsiness, slowed breathing, loss of coordination, and even blackouts. Even one drink with 25mg of Benadryl has led to hospital visits. The FDA requires warning labels on Benadryl packaging specifically about this interaction. Avoid combining them entirely.
Are second-generation antihistamines completely safe with other medications?
Most are much safer, but not risk-free. Loratadine and fexofenadine have minimal interaction potential, but cetirizine still carries a slight anticholinergic burden. If you’re taking strong sedatives like opioids or benzodiazepines, even these can add up. Always check with your pharmacist, especially if you take three or more medications.
Why is Benadryl still sold if it’s so dangerous?
Benadryl is still available because it’s effective for allergies, motion sickness, and short-term sleep aid use. It’s also cheap and widely accessible. But its risks are now well known, and sales have dropped 12.7% per year since 2018. Health organizations recommend avoiding it in favor of safer alternatives, especially for older adults and people on multiple medications.
What’s the safest antihistamine for daily use?
Fexofenadine (Allegra) is currently the safest for daily use. It has no anticholinergic effects, doesn’t interact with liver enzymes, and causes no drowsiness in clinical trials. Loratadine (Claritin) and cetirizine (Zyrtec) are also good options, but cetirizine can cause mild drowsiness in about 10-15% of users. For most people, Allegra is the best choice.
Can antihistamines cause dementia?
Long-term use of high-anticholinergic drugs-including diphenhydramine-is linked to a higher risk of dementia. A 2015 study found people who took these drugs regularly for three years had a 54% increased risk. The American Geriatrics Society now advises avoiding them in older adults for this reason. Switching to low-ACB antihistamines reduces this risk significantly.
How do I know if my medication has anticholinergic effects?
Look up the drug’s ACB score on the University of Washington’s Anticholinergic Burden Calculator. Common anticholinergic drugs include Benadryl (score 3), oxybutynin (3), trazodone (2), and amitriptyline (3). Even some stomach meds and antidepressants carry this risk. If your total score is 3 or higher, talk to your doctor about alternatives.

Nancy Kou
December 21, 2025 AT 09:26Just switched from Benadryl to Allegra last month after nearly passing out at a family BBQ from mixing it with a glass of wine. No more brain fog, no more dizziness, and I actually remember what I ate for dinner. This post nailed it-why do people still think OTC means harmless?
Aadil Munshi
December 22, 2025 AT 22:29Let’s be real-Benadryl isn’t dangerous because it’s a bad drug, it’s dangerous because people treat it like candy. You wouldn’t mix vodka with your Xanax, but you’ll chug a Benadryl and call it ‘just helping me sleep.’ The problem isn’t the medication, it’s the cultural ignorance around CNS depressants. We’ve normalized self-medication to the point where people think ‘natural’ means ‘safe.’ Cetirizine isn’t magic, it’s just science. And if you’re still using diphenhydramine for sleep at 50, you’re not being resourceful-you’re being reckless.
Hussien SLeiman
December 23, 2025 AT 17:11Oh great, another fear-mongering article that ignores context. First-generation antihistamines have been around for 70 years. Millions take them without incident. The 300,000 ER visits? Probably includes people who took 10 pills because they thought it was a ‘sleep hack.’ The real issue isn’t the drug-it’s the people who don’t read labels. And don’t get me started on the ‘dementia link’-correlation isn’t causation. If you take three anticholinergics and drink whiskey every night, yeah, you’re gonna have problems. But blaming Benadryl for your poor life choices is lazy. Also, Allegra costs $15 a bottle. Benadryl is $3. For seniors on fixed incomes, that’s not a trivial difference. Let’s fix the system, not vilify the medicine.
Erica Vest
December 25, 2025 AT 12:37For clarity: The Anticholinergic Cognitive Burden (ACB) scale is validated in peer-reviewed literature and widely adopted by geriatric pharmacists. Diphenhydramine’s ACB score of 3 is consistent across multiple studies, including those from the University of Washington and JAMA. Fexofenadine’s ACB score of 0 is supported by clinical trials showing no significant CNS penetration. The FDA warning labels were added in 2022 after a meta-analysis of 12,000 cases confirmed synergistic respiratory depression. This isn’t opinion-it’s pharmacokinetics.
Kinnaird Lynsey
December 25, 2025 AT 14:02I used to take Benadryl every night for sleep until my mom had a fall and broke her hip. She was on amitriptyline, Benadryl, and a muscle relaxer. Total ACB score: 8. The doctor said she was lucky to be alive. I switched to melatonin and CBT-I. It took two months to adjust, but now I sleep better without feeling like a zombie. This isn’t about fear-it’s about awareness. We don’t need to panic, but we do need to stop pretending OTC means ‘no consequences.’
Glen Arreglo
December 25, 2025 AT 23:52As someone who’s lived in three countries and worked in ERs from Chicago to Bangkok, I’ve seen this play out too many times. In the U.S., people think ‘over-the-counter’ means ‘no prescription needed = no risk.’ In India, they use it like a party drug. In Australia, they don’t even know what it is. The truth? All drugs have risk. The difference is education. We need public health campaigns, not just articles. Pharmacies should have warning stickers on every bottle. Schools should teach basic pharmacology in health class. This isn’t rocket science-it’s basic human safety.
shivam seo
December 27, 2025 AT 19:58Look, I get it. Americans love to over-medicalize everything. Benadryl works. It’s cheap. People use it. If you want to be paranoid about every pill you swallow, go ahead. But don’t act like you’re saving lives by switching to Allegra. I’ve been taking Benadryl with a beer for 15 years. Still breathing. Still driving. Still working. Your ‘science’ is just fear dressed up in lab coats. Let people make their own choices.
benchidelle rivera
December 28, 2025 AT 08:44For anyone reading this who’s ever felt too tired to get out of bed because of a medication combo-this is your sign to talk to your pharmacist. You don’t need to be a genius to understand this. You just need to care enough to ask. I’ve helped over 200 patients in my clinic swap out high-ACB meds. The results? Better sleep, clearer thinking, fewer falls, and less anxiety. It’s not about being perfect. It’s about being informed. And if you’re still using Benadryl as a sleep aid because you think it’s ‘natural’-please, just stop. Your brain will thank you.